ACTUALLY, TWO POSTS HERE: ONE ON MICRO-STRETCHING… OTHER IS LIST A TON OF REFERENCES, ARTICLES, EVIDENCE.
Micro-stretching WORKS… and works very well…IF IT IS DONE RIGHT !!
But most workplaces don’t do this correctly.
You cannot simply Google up a download and tell workers to do them.
THAT DOES NOT WORK!
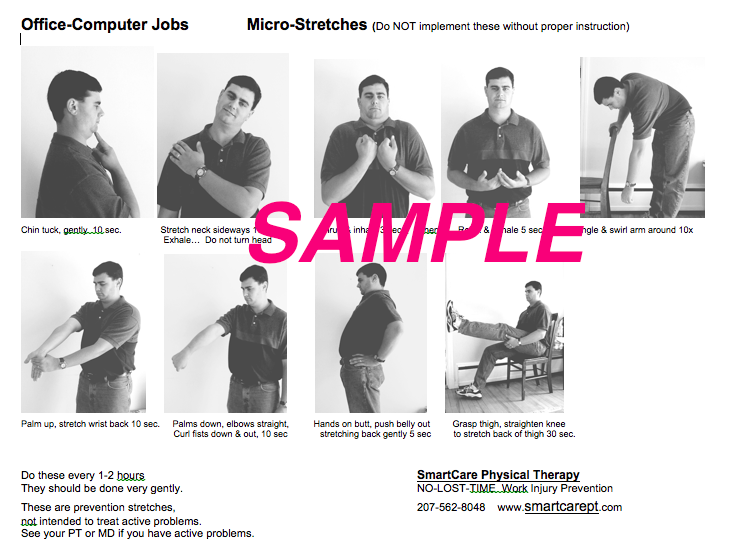
Stretches (or, better yet, microstretches) must be selected to match the MSD risks for the jobs. That can only be done by a professional who is expert on the pathomechanics of MSD (such as the Physical Therapist… the MOST highly trained profesional on this).
Then, employees must be professionally trained: not just on what stretches to do and how to do them, but on WHY… othwise, they won’t do them. Once they understand exactly how each MSD develops and how to reverse that process… then they will commit to doing them.
At least that is our experience at the last 500+ workplaces where we have done this.
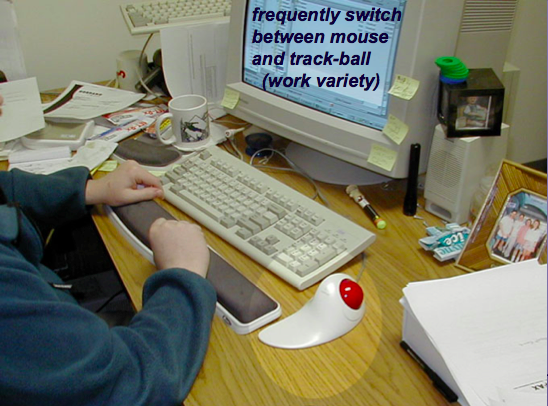
Why workplaces micro-stretching ? … the critical value of micro-stretching? Many jobs have MSD risks that just cannot be engineered away… no ergonomics corrections available. How do we protect these workers? Job task rotation to minimize uninterrupted exposure time… and micro-stretching.
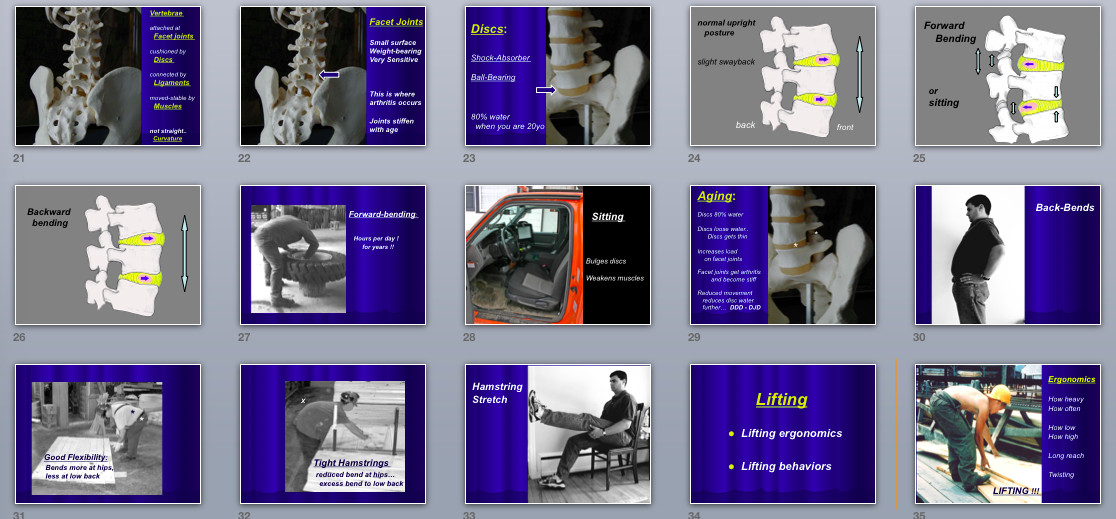
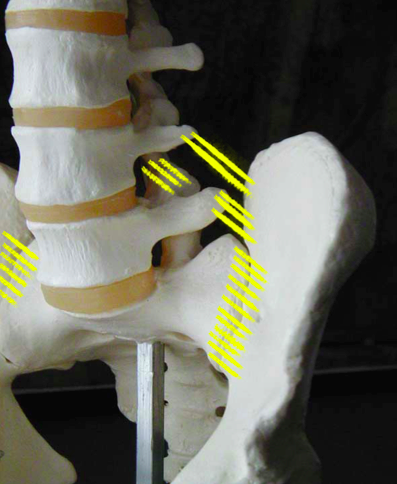
MSD is a nutrient pathway-perfusion problem: When muscles contract, pulling on their tendons, moving or posturing body parts.. they create pressures and tension that exceed the blood pressure feeding those working tissues. That reduces blood flow to working tissues. That allows the waste products of work (acid wastes that become urine) to back up in those tissues, leading to irritation-inflammation and chemical damage… tendinitis, tendinosis, and degeneration of joints and discs.
Ongoing tension or repetitive contractions mechanically inhibit blood flow. Very brief stretches to muscle-tendon groups can create nerve responses (the inhibitory response of the Golgi tendon organs) that relax these tissues, allowing improved blood supply, thus removing irritating and damaging chemical wastes. We are not seeking lengthening of muscles with this particular tactic; just relaxation of the muscle-tendon unit. The objective is to pause loading and relax the built-up background tension, to allow cleansing blood flow to remove metabolic wastes that accumulate and irritate. It also restores coordination and postural awareness.
One major advantage of brief targeted micro-stretches is it offers a prevention tactic that protects workers on jobs that cannot be made harmless through ergonomic modifications (as is so often the case on many jobs).
These may be done as a structured ‘everyone-do-it-together’ routine (less that 2 min total)… or… even better… everyone gets MSD School training teaching what stretches fit what risks and discomforts, so each individual worker will then be self-motivated and skilled at self-selecting stretches to be done whenever they encounter work discomfort (only 10 sec each). This works great.
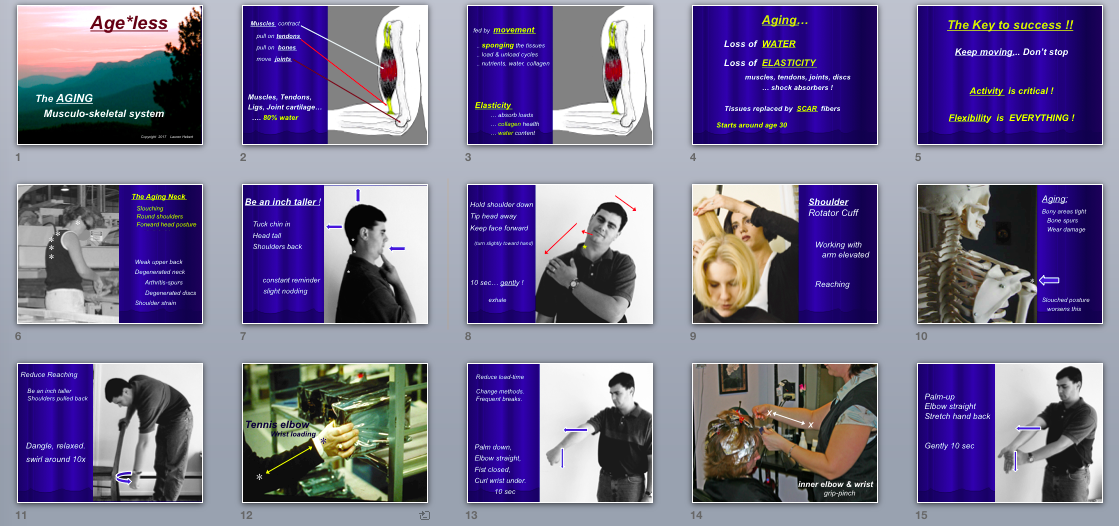
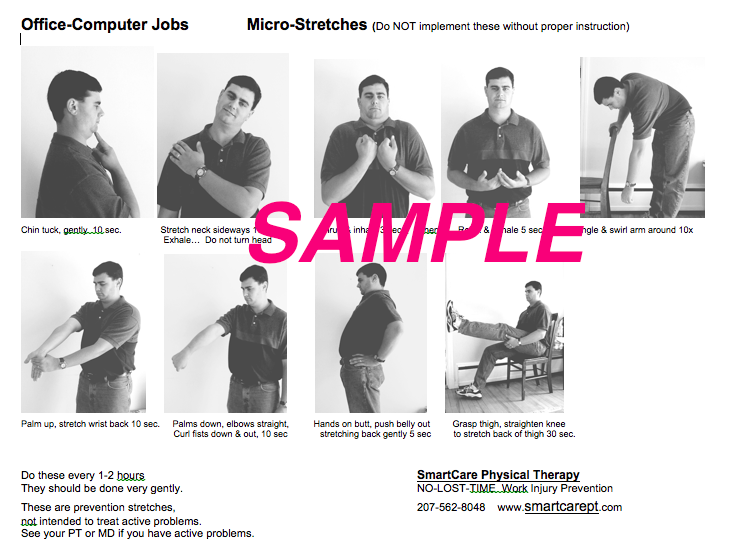
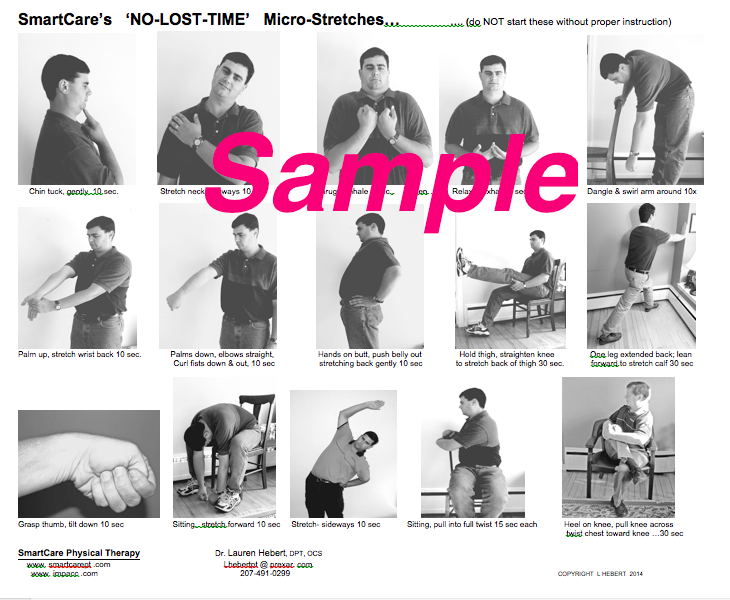
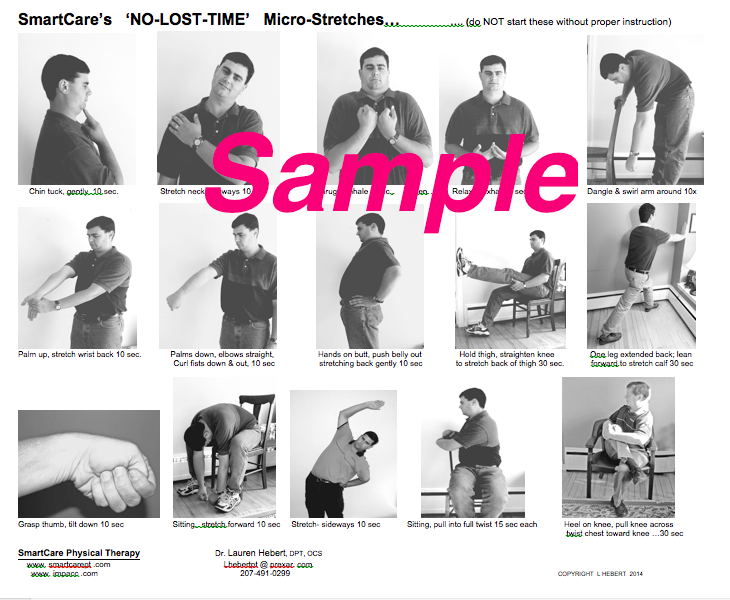
NEW CONCERN… Many companies now employ workplace stretches. But a new problem has appeared: INCORRECT STRETCHES. Here are some at we recommend, because they are specifically targeted to the highest risk body parts.
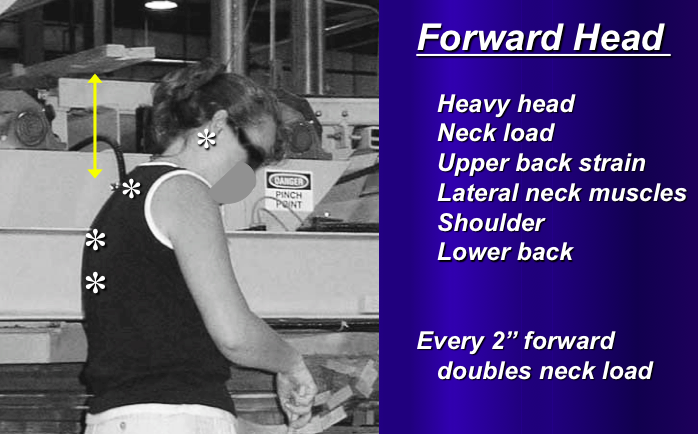
CHIN TUCK stretches the upper spine into a posture that corrects slouching (a severe risk of neck, upper back, and shoulder degeneration).
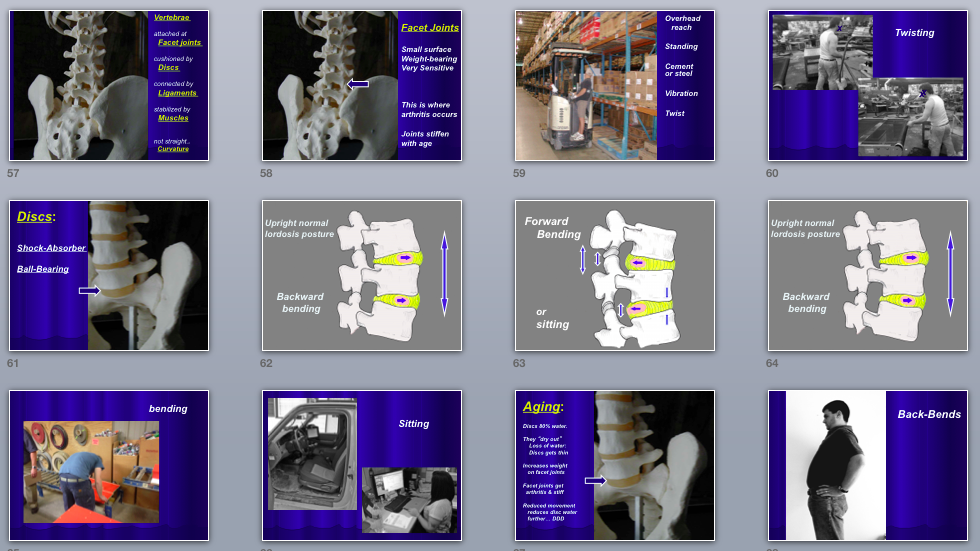
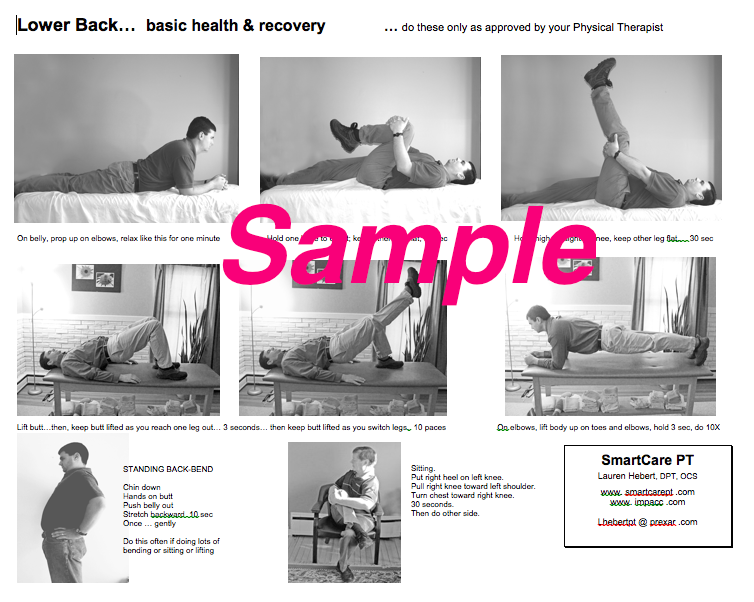
STANDING BACK-BEND stretches lower back into extension, needed for proper disc health and to reduce gradual disc bulging from too much bending or sitting. We recommend the worker flex at neck, not extend head on neck, to moderate spinal forces.
HAMSTRING STRETCH because tight hamstrings reduces hip bending, thus increasing bending loads on the vulnerable lower back, risking disc herniation and degeneration.
LATERAL NECK SCALENI STRETCHES because sitting and slouch allows later neck muscles to tighten, compressing blood vessels and nerves that pass through them on their way to the arm and carpal tunnel. Common error is allowing rotation to occur during sidebending stretch.
SHOULDER CODMAN-PENDULUM for jobs with reaching, loading rotator cuff tendons. This greatly relaxes cuff and restores blood supply to shoulder muscles.
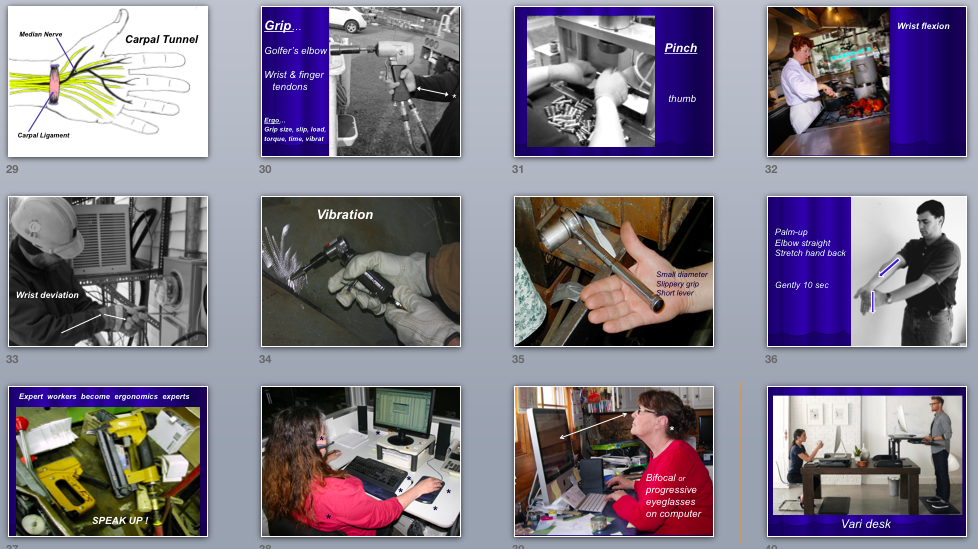
TENNIS ELBOW STRETCH is often done incorrectly in many workplaces. This must stretch both wrist and finger extensors that usually lose elasticity from over-use. This micro-stretch restore blood supply and elasticity here. Common error is stretching into wristflexion with fingers open-neutral… NOT correct…should be done with fist closed to include digit extensors in the stretch, since they share that proximal tendon and are part of radial tunnel.
GOLFER’S ELBOW & CARPAL TUNNEL STRETCH is also often done incorrectly by many workplaces. This is to stretch wrist-finger flexors (grip and pinch work) PLUS the pronator muscle at the front-to-inside of forearm-elbow, responsible for stressing inner elbow and squeezing nerves to carpal tunnel. Common error is doing this stretch with forearm pronated… NOT correct… forearm should be supinated to include pronator teres in the stretch, since that is a source of median nv entrapment adding to CTS risk.
DEQUERVAIN’S–THUMB STRETCH addresses work tasks that use thumb loads.
CALF STRETCH reduces plantar fasciitis heel spur and achilles tendon risks.
There may be others, customized to specific jobs (middle back torsion for forklift drivers, others for maintenance tasks, e.g.).
Stretch programs should be designed by a professional Physical Therapist with knowledge of the jobs… to design a small, practical, targeted program.. that is taught to employees by that PT to motivate employee acceptance and skills in these. The key is face to face training in an MSD School format that teaches not only what to do, but WHY to do it… or else they won’t do it at all.
THAT IS WHY WE DO NOT POST A DOWNLOAD OF OUR MICRO-STRETCHES
Here is one version customized for office setting (with a blocking overlay to inhibit download use). Other versions customized for other settings, e.g., warehouse materials handling work, repetitive task mfg, etc.
Office format of micro-stretching
Wider workplace demands micro-stretch program
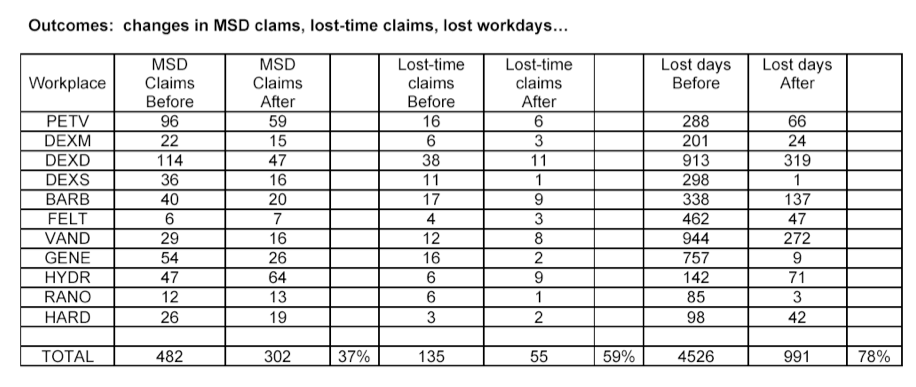
OUR OUTCOMES… Table of data from a study we did of our outcomes, published in Ortho APTA’s monograph self-study course “The Injured Worker” encompassing several thousand workers in multiple states trained by several PT’s using the same MSD School program and micro-stretch protocol. Claims reduced 37%; lost time claims reduced 59%; MSD lost days reduced 78%.
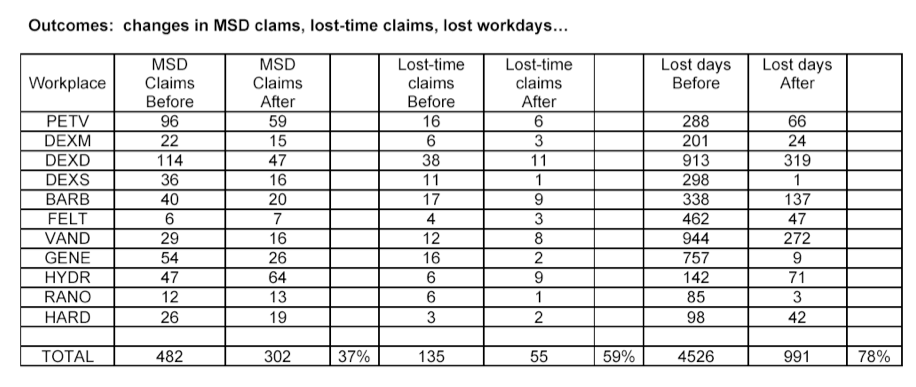
Workplace stretching has historically been controversial. But it has been rather conclusively shown to be highly effective… if it is done right. Our practice is perhaps the MOST experienced of all entities on this topic. Yes, it does work, very well, if done right (many do it wrong, even some PTs). You can find evidence summarized at our prevention site at http://www.impacc.com .
What is the critical value of micro-stretching? Many jobs have MSD risks that cannot be re-engineered away… no ergonomics corrections available. How do we protect these workers? Job task rotation to minimize uninterrupted exposure time… and micro-stretching.
Micro-stretching is a concise collection of very brief 10-second stretches that specifically target muscle-tendon-joint units that are exposed to the MSD risk. But ten seconds is not prolonged enough to lengthen tight soft tissues, right? Probably so. But that is not what we seek. We seek a relaxation of the overworked muscle-tendon unit, to allow a restoration of tissue perfusion. Repeated or sustained contraction blocks tissue perfusion, causing anaerobic metabolism causing buildup of metabolic wastes, which stimulate inflammation. Ten seconds mild sustained stretch stimulates Golgi Tendon Organs (remember those?) which then inhibit spindle activity… relaxing the contractile unit, allowing perfusion to pour through.
For 30 years we have been badgering employers to implement stretching. Most have now done so. But most are doing it incorrectly. Example: tennis elbow stretch has elbow straight, forearm pronated, wrist flexed down toward floor, person uses other hand to stretch wrist into full flexion. Right” Nope. Place your own arm in this position and ‘feel’ the stretch. Now, one simple change: close your fingers into a fist. Feel the change? Much more of a stretch now. The extensor digitorum shares the origin of the ECR muscle and is often part of tennis elbow and radial tunnel compression. This is the correction: do the tennis elbow stretch with fingers closed, for much more effective stretch.
Another example is stretching wrist-digit flexors to prevent CTS and wrist tendinitis. Most do this with elbow straight, forearm pronated, stretch hand into extension. Try this on yourself and ‘feel’ the stretch. BUT… try it with forearm in supination instead of pronation. Feel the difference? It is much more effective done in supination than in pronation… because we need to stretch the pronator teres in this stretch… to reduce pronator compression of median nerve (a risk factor for CTS or median nv compress at pronator) and reduce risks of medial epicondylalgia. This is another important correction for reducing workplace MSD through micro-stretching.
We also see an epidemic of including too many stretches in a program. That raises risk of improper stretching or abandoning stretching altogether. I see this error among PTs in the clinic. Give people the lowest number of exercises needed to gain accurate compliance. A typical microstretch program usually consists of only 8 stretches, customized to the job. Companies need a concises program that does not consume more than 3-5 minutes… or else it won’t happen at all.
Also we include stretches at neck to reduce forward head and tight thoracic outlet. Many workplace neglect the neck role in UE MSD risks.
MicroStretching may occur on a structured schedule such as at start of shift, return from each greak… but even more effective, employees should be professionally trained to self-select stretches whenever they notice discomfort to target relief to the affected body part. The key to this is excellent employee education by the PT expert.
Another effective component is a concise set of after-work recovery stretches.
Always include a disclaimer! “These exercises are prevention and wellness stretches. if you already have problems, consult your own PT to approve or modify stretches that are proper for you. Do NOT start doing any stretches without professional instruction by a physical therapist.”
And please, do NOT post your stretch programs online for people to download. You would not do that with clinic-based back exercises, right? Why? Because not everyone needs the same stretches. You would not want someone with disc herniation doing sit-ups and crunches and bilateral flexions stretches, right? And you don’t want someone with grade 4 spondylolisthesis doing prone pressups, right? Same with workplace stretches. They need (1) to be customized to the job risks and (2) people must be professionally instructed how and WHY to do each stretch, to assure safe execution.
————————————————————————————
IMPORTANT….
REFERENCES, EVIDENCE, BIBLIOGRAPHY… (for all our tactics)
1.Bureau of Labor Standards: incidence and costs of MSD. http://www.bls.gov/news.release/osh2.nr0.htm. Accessed February 6, 2013.
2.Congressional testimony by OSHA director on proposed OSHA ergonomics standards.
http://www.osha.gov/pls/oshaweb/owadisp.show_document?p_id=166&p_table=TESTIMONIES. Accessed February 7, 2013.
3.APTA Vision Sentence 2020.
http://www.apta.org/vision2020/. Accessed February 8, 2013.
4.Pillastrini P, Mugnai R, Farneti C, Bertozzi L, Bonfiglioni R, Curti S, et al. Evaluation of two preventive interventions for reducing musculoskeletal complaints in operators of video display terminals. Phys Ther. 2007;78(5):536-543.
5.Ries E. Working solutions: PT’s and ergonomics. PT Magazine. 2004;12(9):38-44.
6.Hebert L. Becoming a consultant to industry. Ortho PT Pract. 2000;12(20):12-14.
7.Hebert L. Preventive stretching exercises for the workplace, Ortho PT Pract. 1999;11(4):11-12.
8.Hebert, L. Analytic focus reduces anxiety over CTD claims, J Occ Health and Safety. 1993;62(4):56-62.
9.OSHA Ergonomics Program Final Rule. http://www.osha.gov/pls/oshaweb/owadisp.show_document?p_table=federal_register&p_id=16305. Accessed February 9, 2013.
10.OSHA. CFR Part 1910 Ergonomics Program Federal Register. Vol. 64, No 225. 1999: Occupational Safety and Health Administration, U.S. Dept of Labor.
11. OSHA ergonomic program management guidelines for industry sectors. http://www.osha.gov/SLTC/ergonomics/guidelines.html. Accessed February 9, 2013.
PATHOPHYSIOLOGY OF M.S.D.
12.Barr A, Barbe M. Pathophysiological tissue changes associated with repetitive movement: a review of the evidence. Phys Ther. 2002;82(2):173-187.
13.Barr AE, Barbe MF, Clark BD. Work-related musculoskeletal disorders of the hand and wrist: epidemiology, pathophysiology, and sensorimotor changes. J Orthop Sports Phys Ther. 2004;34(10):610-627.
14.Byl NN, Merzenich MM, Cheung S, Bedenbaugh P, Ngarajan SS, Jenkins WM. A primate model for studying focal dystonia and repetitive strain injury: effects on the primary motor cortex. Phys Ther. 1997;77(3):269-284.
15.Fernandez-de-las-Penas C, Ortega-Santiago R, Ambite-Quesada S, Jimenez-Garcia R, Arroyo-Morales M, Cleland JA. Specific mechanical pain hypersensitivity over peripheral nerve trunks in women with either unilateral epicondylalgia or carpal tunnel syndrome. J Orthop Sports Phys Ther. 2010;40(11):751-760.
16.Luopajarvi T. Ergonomic analysis of workplace and postural load. In: Bullock M, ed. Ergonomics: The Physiotherapist in the Workplace. New York, NY: Churchill Livingstone; 1990:51-78.
17.Grozdanovic M. Human activity and musculoskeletal injuries and disorders. Facta Universitatis Series Medicine and Biology. 2002;9,(2):150-156.
18.Rees JD, Wilson AM, Wolman RL. Current concepts in the management of tendon disorders. Rheumatology. 2006;45(5):508-521.
19.Rees JD, Maffulli N, Cook J. Management of tendinopathy. Am J Sports Med. 2009;37(9):1855-67.
20.Cook JL, Purdam CR. Is compressive load a factor in the development of tendinopathy? Br J Sports Med. 2012;46:163-168.
21.Cook JL, Purdam C. Is tendon pathology a continuum? A pathology model to explain the clinical presentation of load-induced tendinopathy. Br J Sports Med. 2009;43;409-416.
22.Nee RJ, Butler D. Management of peripheral neuropathic pain: Integrating neurobiology, neurodynamics, and clinical evidence. Phys Ther Sport. 2006;7(1):36-49.
23.Baron R. Mechanisms of Disease: neuropathic pain—a clinical perspective. Nature Clinical Practice Neurology. 2006;2:95-106.
24.Butler DS. Pain mechanisms and peripheral sensitivity. In: The Sensitive Nervous System. Adelaide, Australia: Noigroup Publ; 2000:47-71.
25.Strong J, Unruh AM, Wright A, Baxter GD: Neurophysiology of pain and pain modulation. In: Pain: A textbook for therapists. London: Elsevier Churchill Livingstone; 2002:43-64.
26.Shacklock M. General neuropathodynamics. In: Clinical Neurodynamics. London: Elsevier; 2005:59-72.
27.Iridiastadi H, Nussbaum MA. Muscle fatigue and endurance during repetitive intermittent static efforts: development of prediction models. Ergonomics. 2006;49(4):344-60.
28.Visser B, Jaap H, van Dieen. Pathophysiology of upper extremity muscle disorders. J Electromyography Kinesiol. 2006;16(1):1-16.
29.Roquelaure Y, Rouillon C, Fouquet N, LeclercA, Descatha A, Touranchet A, et al. Risk factors for upper-extremity musculoskeletal disorders in the working population. Arthritis Rheum. 2009 Oct 15;61(10):1425-34.
30.Sembajwe G, Wahrendorf M, Siegrist J, Sitta R, Zins M, Goldberg M, Berkman L. Effects of job strain on fatigue: cross-sectional and prospective views of the job content questionnaire and effort–reward imbalance in the GAZEL cohort. Occup Environ Med. 2012;69:377-384.
31.Barbe MF, Barr AE. Inflammation and the pathophysiology of work-related musculoskeletal disorders. Brain, Behavior, and Immunity. 2006;20(5):423-29.
32.Walker-Bone K, Cooper C. Hard work never hurt anyone: or did it? A review of occupational associations with soft tissue musculoskeletal disorders of the neck and upper limb. Ann Rheum Dis. 2005;64:1391-96.
33.Van Rijn RM, Huisstede BM, Koes BW, Burdorf A. Associations between work-related factors and specific disorders at the elbow: a systematic literature review. Rheumatology (Oxford). 2009;48(5):528-36.
34.Mehta RK, Agnew MJ. Influence of mental workload on muscle endurance, fatigue, and recovery during intermittent static work. Eur J Appl Physiol. 2012;112(8):2891-902.
35.Larsman P, Hanse JJ. A longitudinal path model of psychological workload, fatigue and neck/shoulder symptoms among female childcare workers. Work. 2009;32(2):219-26.
36.McPhee B. Musculoskeletal complaints in workers engaged in repetitive work in fixed postures. In: Bullock M, ed. Ergonomics: The Physiotherapist in the Workplace. New York, NY: Churchill Livingstone; 1990:101-132.
37.Twoney LT. A rationale for the treatment of back pain and joint pain by manual therapy. Phys Ther. 1992;72(12):885-892.
38.Porterfield JA, DeRosa C. Mechanical Low Back Pain. Philadephia PA: WB Saunders; 1998:121-167.
39.Hashimoto T, Nobuhara K, Hamada T. Pathologic evidence of degeneration as a primary cause of rotator cuff tear. Clin Ortho Relat Res. 2003;(415):111-120.
40. Blain E, Zhang Y, Aeschlimann D, Caterson B, Duance V. Changes in tendon extracellular matrix composition with age. Int J Exp Path. 2004;85(1):A33-A34.
M.S.D. RISK FACTORS…
41.Novak CB. Upper extremity work-related musculoskeletal disorders: a treatment perspective. J Orthop Sports Phys Ther. 2004;34(10):628-637.
42.Harms-Ringdahl K, Schuldt K. Neck and shoulder load and load-elicited pain in sitting work postures. In: Bullock M, ed. Ergonomics: The Physiotherapist in the Workplace. New York, NY: Churchill Livingstone; 1990:133-147.
43.De-le-Rincon AI, Palacios-Cena D, Fernandez-de-las-Penas C, Cleland JA. Increased forward head posture and restricted cervical range of motion in patients with carpal tunnel syndrome. J Orthop Sports Phys Ther. 2009:39(9);658-664.
44.Prizinski F, Brence J. Effective treatment of bilateral carpal tunnel symptoms using cervicothoracic thrust manipulation, neural glides, and periscapular strengthening: a case report. Orthopaedic Practice. 2011;23(2):84-88.
45.Lee MJ, LaStayo PC. Pronator syndrome and other nerve compressions that mimic carpal tunnel syndrome. .J Orthop Sports Phys Ther. 2004;34(10);601-609.
46.Edgelow P. Neurovascular consequences of cumulative trauma disorders affecting the thoracic outlet. In: Donatelli R, ed. Physical Therapy of the Shoulder. New York NY; Churchill Livingstone.1997:153-178.
47.Pascarelli EF, Hsu YP. Understanding work-related upper extremity disorders: clinical findings in 485 computer users, musicians, and others. J Occup Rehabil. 2001 Mar;11(1):1-21.
48.Vaught MS, Brismee JM, Dedrick GS, Sizer PS, Sawyer SF. Association of disturbances in the thoracic outlet in subjects with carpal tunnel syndrome: a case-control study. J Hand Ther. 2011 Jan-Mar;24(1):44-51.
49.Lo SF, Chou LW, Meng NH, Chen FF, Juan TT, Ho WC, Chiang CF. Clinical characteristics and electrodiagnostic features in patients with carpal tunnel syndrome, double crush syndrome, and cervical radiculopathy. Rheumatol Int. 2012 May;32(5):1257-63.
50.Van Rijn RM, Huisstede BM, Koes BW, Burdorf A. Associations between work-related factors and specific disorders at the shoulder: a systematic review of the literature. Scand J Work Environ Health. 2010;36(3):189-201.
51.Roquelaure Y, Bodin J, Ha C, Petit Le Manac’h A, Descatha A, Chastang JF, et al. Personal, biomechanical, and psychosocial risk factors for rotator cuff syndrome in a working population. Scand J Work Environ Health. 2011;37(6):502-11.
52.Ciccltti MC, Schwartz MA, Ciccotti MG. Diagnosis and treatment of medial epicondylitis of the elbow. Clin Sports Med 23 (2004); 693-705.
53.Descatha A, Leclerc A, Chastang JF, Roquelaure Y. Medial epicondylitis in occupational settings: prevalence, incidence and associated risk factors. J Occup Environ Med. 2003;45(9):993-1001.
54.Descatha A, Leclerc A, Chastang JF, Roquelaure Y. Incidence of ulnar nerve entrapment at the elbow in repetitive work. Scand J Work Environ Health. 2004;30(3):234-40.
55.Van Rijn RM, Huisstede BM, Koes BW, Burdorf A. Associations between work-related factors and the carpal tunnel syndrome: a systematic review review. Scand J Work Environ Health. 2009;35(1):19-36.
56.Petit Le Manac’h A, Roquelaure Y, Ha C, Bodin J, Meyer G, Bigot F, et al. Risk Factors for de Quervain’s disease in a French working population. . Scand J Work Environ Health. 2011;37(5):394-401.
57. Byng J. Overuse syndromes of the upper limb and the upper limb tension test: a comparison between patients, asymptomatic keyboard workers and asymptomatic non-keyboard workers. Man Ther. 1997;2(3):157-164.
LOW BACK MSD RISK FACTORS…
58.McKenzie RA, May S. The Lumbar Spine: Mechanical Diagnosis and Therapy. Waikanae NZ: Spinal Publications; 2003.
59.Cyriax J. Textbok of Orthopaedic Medicine, Vol 1. Baltimore Md: Williams and Wilkins;1975:444-451.
60.Nachemson AL. Disc Pressure measurements. Spine. 1981;6(1):93-7.
61.Popovich JM Jr, Welcher JB, Hedman TP, Tawackoli W, Anand N, Chen TC, Kulig K. Lumbar facet joint and intervertebral disc loading during simulated pelvic obliquity. Spine J. 2013. Epub ahead of print. http://www.ncbi.nlm.nih.gov/pubmed/23706384. Accessed June 2, 2013.
62.Bovajian-O’Neil LA, McCain RL, Coleman MK, Thomas PP. Diagnosis and management of piriformis syndrome: an osteopathic approach. J Am Osteopath Assoc. 2008;108(11):657-64.
63.Tonley JC, Yun SM, Kochever RJ, Dye JA, Farrokhi S, Powers CM. Treatment of an individual with piriformis syndrome focusing on hip uscle strengthening and movement reeducation: a case report. J Orthop Sports Phys Ther. 2010;40(2):103-111.
64.Porterfield JA, DeRosa C. Mechanical Low Back Pain. Philadephia PA: WB Saunders; 1998:148-164.
65.Massoud Arab A, Reza Nourbakhsh M, Mohammadifar A. The relationship between hamstring length and gluteal muscle strength in individuals with sacroiliac joint dysfunction. J Man Manip Ther. 2011;19(1):5-10.
66.Porterfield JA, DeRosa C. Mechanical Low Back Pain. Philadephia PA: WB Saunders; 1998:21-22.
67.Childs JD, Teyhen DS, Casey PR, McCoy-Singh KA, Feidltmann AW, Wright AC, et al. Effects of traditional sit-up training versus core stabilization exercises on short-term musculoskeletal injuries in US Army soldiers: a cluster randomized trial. Phys Ther. 2010;90(10):1404-12.
68.Inani SB, Selkar SP. Effect of core stabilization exercises versus conventional exercises on pain and functional status in patients with non-specific low back pain: a randomized clinical trial. J Back Musculoskelet rehabil. 2013;26(1):37-43.
69.Borghuis J, Hof AL, Lemmink LA. The importance of sensory-motor control in providing core stability: implications for measurement and training. Sports Med. 2008;38(11):893-916.
70.Barr KP, Griggs M, Cadby T. Lumbar stabilization: a review of core concepts and current literature, part 2. Am J Phys Med Rehabil. 2007;86(1):72-80.
71.Standaert CJ, Herring SA. Expert opinion and controversies in musculoskeletal and sports medicine: core stabilization as a treatment for low back pain. Arch Phys Med Rehabil. 2007;88(12):1734-6.
72.Jarvik JG, Hollingworth W, Heagerty PJ, Haynor DR, Boyko EJ, Deyo RA. Three-year incidence of low back pain in an initially asymptomatic cohort: clinical and imaging risk factors. Spine. 2005;30(13):1541-8.
73.MacEachen E, Kosny A, Ferrier S, Chambers L. The “toxic dose” of system problems: why some injured workers don’t return to work as expected. J Occup Rehabil. 2010;20(3):349-66.
74. Baril R, Clarke J, Friesen M, Stock S, Cole D. Management of return-to-work programs for injured workers with musculoskeletal disorders: a qualitative study in three Canadian provinces. Soc Sci Med. 2003;57(11):2101-14.
BACK SCHOOL EVIDENCE…
75. Nelson A, Matz M, Chen F, Siddharthan K, Lloyd J, Fragala G. Development and evaluation of a multifaceted ergonomics program to prevent injuries associated with patient handling tasks. Int J Nurs Stud. 2006;43(6):717-33.
76.Lee TH, Huang SM. Effects of wrist rest and forearm support on muscle activity. Perceptual and Motor Skills. 2006;103(3):873-878.
77.Hasegawa T, Inoue K, Tsutsue O, Kumashiro M. Effects of a sit-stand schedule on a light repetitive task. Int J Indust Ergo. 2001;28(3-4):219-224.
78.Schenk RJ, Doran RL, Stachura JJ. Learning effects of a back education program. Spine. 1996;21(19):2183-8; discussion 2189.
79.Holmes W, Lam PY, Elkind P, Pitts K. The effect of body mechanics education on the work performance of fruit warehouse workers. Work. 2008;31(4):461-71.
80.Gatty CM, Turner M, Buitendorp DJ, Batman H. The effectiveness of back pain and injury prevention programs in the workplace. Work. 2003;20(3):257-266.
81.Daltroy LH, Iverson MD, Larson MG, Lew R, Wright E. A controlled trial of an education program to prevent low back injuries. NE J Med. 1997;337(5):323-328.
82.Karas BE, Conrad KM. Back injury prevention in the workplace: an integrative review. AAOHN. 1996;44(4):189-96.
83.Linton SJ, Kamwendo K. Low back schools: a critical review. Phys Ther. 1987;67:1375-1383.
84.Versloot JM, Rozeman A, van Son AM, van Akkerveeken PF. The cost-effectiveness of a back school program in industry: a longitudinal controlled field study. Spine. 1992;17(1):22-7.
85. Heymans MW, van Tulder MW, Esmail R, Bombarier C, Koes BW. Back schools for nonspecific low back pain: a systematic review within the framework of the Cochrane collaboration back review group. Spine. 2005;30(19):2153-63.
ERGO ASSESSMENT TOOLS…
86.Snook SH, Ciriello VM. The design of manual handling tasks: revised tables of maximum acceptable weights and forces. Ergonomics. 1991;34(9)1197-1213.
87.Liberty Mutual manual materials handling tables. http://libertymmhtables.libertymutual.com/CM_LMTablesWeb/taskSelection.do?action=initTaskSelection. Accessed January 26, 2013.
88.Waters TR, Putz-AndersonV, Grag A. Applications Manual for the Revised NIOSH Lifting Equation. US Department of Health and Human Services; Public Health Service; NIOSH. 1994.
89.Online version of the Application Manual for the Revised NIOSH Lifting Equation
http://wonder.cdc.gov/wonder/prevguid/p0000427/p0000427.asp. Accessed June 4, 2013.
90.NIOSH Lifting Equation online calculator.
http://www.emcins.com/losscontrol/quick_links/employee_safety_health/ergonomicsNIOSH.aspx. Accessed January 26, 2013.
91.Online instructions for calculating NIOSH Lifting Equation Composite Lifting Index for multiple-task lifting jobs.
http://www.ergo-plus.com/healthandsafetyblog/ergonomics/niosh-lifting-equation-multiple-tasks. Accessed June 4, 2013.
92.WISHA Lifting Analysis tool. http://www.lni.wa.gov/wisha/ergo/evaltools/ergocalc.pdf. Accessed January 26, 2013.
93.WISHA Lifting Analysis tool and quick checklist.
http://personal.health.usf.edu/tbernard/HollowHills/WISHA_Lifting.pdf. Accessed January 26, 2013:
OTHER ERGO ANALYSIS; REBA; RULA, ETC…
94.McAtamney L, Corlett EN. RULA: a survey method for the investigation of work-related upper limb disorders. Applied Ergonomics. 1993;24(2):91-99.
95.RULA analysis worksheet. http://ergo.human.cornell.edu/Pub/AHquest/RULAworksheet.pdf. Accessed January 26, 2013.
96.Hignett S, McAtamney L. Rapid entire body assessment (REBA). Applied Ergonomics.2000;31:201-205.
97.REBA analysis worksheet. http://personal.health.usf.edu/tbernard/HollowHills/REBA.pdf. Accessed January 26, 2013.
98.Online lessons on how to perform REBA and RULA. http://www.ncsu.edu/ehs/www99/right/handsMan/office/RULA_REBA_Presentation.pdf. Accessed January 26, 2013.
99.Online lessons on how to perform REBA and RULA.
http://www.ergo-plus.com/healthandsafetyblog/ergonomics/reba-assessment-tool-guide/. Accessed January 26, 2013
100.SAFE Manitoba Ergonomics Risk Factors Checklist. http://safemanitoba.com/uploads/ergonomicriskfactorchecklist.doc
This is a download document linked from:
http://safemanitoba.com/search/apachesolr_search/ergonomics%20checklist.
Accessed January 26, 2013.
101.OSHA 300 log recordkeeping guidelines. http://www.osha.gov/recordkeeping/new-osha300form1-1-04.pdf. Accessed January 26, 2013.
102.Bernacki EJ, Guidera JA, Schaefer JA, Tsai S. A facilitated early return to work program at a large urban medical center. J Occup Environ Med. 2000;42:1172-1177.
103.Haukka E, Leino-Arjas P, Viikari-Juntura E et al. A randomized controlled trial on whether a participatory ergonomics intervention could prevent musculoskeletal disorders. Occup Environ Med. 2008;65(12):849-56.
104.Zeydi IM, Heydarnia A, Niknami S. The prediction of adoption with correct sitting postural habit: an application of the theory of planned behavior. Eur J Sci Res. 2009;29(2):205-214.
105. OSHA’s suggested Ergonomic Program Management Guidelines 3123. http://www.osha.gov/Publications/OSHA3123/3123.html. Accessed February 17, 2013.
FOREARM SURFACE REST-SUPPORT AS AN ERGO TACTIC…
106.Rempel DM, Krause R, Goldberg R, et al. A randomized controlled trial evaluating the effects of two workstation interventions on upper body pain and incidents musculoskeletal disorders among computer operators. Occup Environ Med. 2006;63:300-306.
107. Cook C, Burgess-Limerick R, Papalia S. The effect of upper extremity support on upper extremity posture and muscle activity during keyboard use. Applied Ergonomics. 2004;35(3):285-92.
108. Lee TH, Huang SM. Effects of wrist rest and forearm support on muscle activity. Perceptual and Motor Skills. 2006;103(3):873-878.
109. Lee TH, Huang SM. Effects of wrist rest and forearm support on muscle activity. Perceptual and Motor Skills. 2006;103(3):873-878.
11oA. Cook C, Downse L, Bowman J. Long-term effects of forearm support: computer users working at conventional desks. Work. 2008;30(2):107-112.
110B Nag PK, Pal S, Nag A, Vyas H. Influence of arm and wrist support on forearm and back muscle activity in computer keyboard operation. Applied Ergonomics. 2008; 40(2):286-291.
SIT-STAND OPTIONS AS AN ERGO TACTIC…
111A. Husemann B, Von Mach CY, Borsotto D, Zepf KI, Scharnbacher J. Comparisons of musculoskeletal complaints and data entry between a sitting and a sit-stand workstation paradigm. Hum Factors. 2009;51(3):310-20.
111B. Hasegawa T, Inoue K, Tsutsue O, Kumashiro M. Effects of a sit-stand schedule on a light repetitive task. Int J Indust Ergo. 2001;28(3-4):219-224.
112. Robertson MM, Ciriello VM, Garabet AM. Office ergonomics training and a sit-stand workstation: effects on musculoskeletal and visual symptoms and performance of office workers. Appl Ergon. 2013;44(1):73-85
113.Alkhajah TA, Reeves MM, Eakin EG, Winkler EA, Owen N, Healy GN. Sit-stand workstations: a pilot intervention to reduce office sitting time. Am J Prev Med. 2012;43(3):298-303.
114.Pronk NP, Katz AS, Lowry M, Payfer JR. Reducing occupational sitting time and improving worker health: the Take-a-Stand Project, 2011. Prev Chronic Dis. 2012;9:154.
115.Callaghan JP, McGill SM. Low back joint loading and kinematics during standing and unsupported sitting. Ergonomics. 2001;44(3):280-94.
116.Cagnie B, Danneels L, Van Tiggelen D, De Loose V, Cambier D. Individual and work related risk factors for neck pain among office workers: a cross sectional study. Eur Spine J. 2007;16(5):679-86.
117.Dankaerts W, O’Sullivan P, Burnett A, Straker L. Differences in sitting postures are associated with nonspecific chronic low back pain disorders when patients are subclassified. Spine. 2006;31(6):698-704.
118.posture changes McLean L. The effect of postural correction on muscle activation amplitudes recorded from the cervicobrachial region. J Electromyogr Kinesiol. 2005;15(6):527-35.
119. Balci R, Aghazadeh F:The effects of work-rest schedules and type of task on the discomfort and performance of VDT users. Ergonomics. 2003;46(5):455-65
120.OSHA recommendations for computer work MSD prevention. http://www.osha.gov/SLTC/etools/computerworkstations/workprocess.html#Prolonged. Accessed February 6, 2013.
121.Office Ergonomics: practical solutions for a safer workplace
Washington State Dept of labor and Industries, WISHA Services Division
http://www.lni.wa.gov/IPUB/417-133-000.pdf . Accessed 6/13/2013
OTHER ERGO TACTICS… JOB ROTATIONS, ETC…
122.Bidassie B, McGlothlin JD, Goh A, Feyen RG, Barany JW. Limited economic evaluation to assess the effectiveness of a university-wide office ergonomics program. Appl Ergon. 2010;41(3):417-27.
123.Marklin RW, Simoneau GC. Design features of alternative computer keyboards: a review of experimental data. J Orthop Sports Phys Ther.. 2004;34(10):638-649.
124.Norlander C, Ohlsson K, Akesson I, Arvidsson I, Balogh I. Hansson GA, et al. Risk of musculoskeletal disorders among females and males in repetitive/constrained work. Ergonomics. 2009;52(10):1226-39.
125.Horton LM, Nussbaum MA, Agnew MJ. Effects of rotation and task order on localized muscle fatigue and performance during repetitive static shoulder exertions. Ergonomics. 2012;55(10):1205-17.
126.Davis K, Jorgensen M. Ergonomics. Pros and cons of job rotation as a means of reducing injury costs. J Occup Environ Hyg. 2005;2(1):D1-3.
127.Melhorn JM. A prospective study for upper extremity cumulative trauma disorders of workers in aircraft manufacturing. J Occup Enviorn Med. 1996 Dec;38(12):1264-71.
128.Goodman G, Kovach L, Fisher A, Elsesser E, Bobinski D, Hansen J. Effective interventions for cumulative trauma disorders of the upper extremity in computer users: practice models based on systematic review. Work. 2012;42(1):153-72.
129.Delitto RS, Rose SJ. An electromyographic analysis of two lifting techniques for squat lifting and lowering. Phys Ther. 1992;72(6):438-48
130.Hart DL, Stobbe TJ, Laraiedi M. Effect of lumbar posture on lifting. Spine. 1987;12(2):138-145.
131.Kingma I, Faber GS, van Dieen JH. How to lift a box that is too big to fit between the knees. Ergonomics. 2010;53(10):1228-38.
132.Bazrgari B, Shirazi-Adl A, Arjmand N. Analysis of squat and stoop dynamic liftings: muscle forces and internal spinal loads. Eur Spine J. 2007;16(5):687-99.
133.Linton SJ, van Tulder MW. Preventive interventions for back and neck pain problems. Spine. 2001;26(7):778-787.
134.Moore TM. A workplace stretching program. Physiologic and perception measurements before and after participation. AAOHN J. 1998 Dec;46(12):563-8.
135.Fenety A, Walker JM. Short-term effects of workstation exercises on musculoskeletal discomfort and postural changes in seated video display unit workers. Phys Ther. 2002;82(6):578-589.
136.Jepson JR, Thomsen G. Prevention of upper limb symptoms and signs of nerve afflictions in computer operators: the effects of intervention by stretching. J Occup Med Toxicol. 2008;3(1).
137. daCosta BR, Vieira ER. Stretching to reduce work-related musculoskeletal disorders: a systematic review. J Rehabil Med. 2008;40:321-328.
** WORKPLACE STRETCHING FOR MSD PREVENTION…
138.Hebert L. Preventive stretching exercises for the workplace, Ortho PT Pract. 1999;11(4):11-12.
139 Marangoni AH. Effects of intermittent stretching exercises at work on musculoskeletal pain associated with the use of a personal computer and the influence of media on outcomes. Work. 2010;36(1):27-37.
140.Barredo RD, Mahorn K. The effects of exercise and rest breaks on musculoskeletal discomfort during computer tasks: an evidence-based perspective. J Phys Ther Sci. 2007;19(2):151-163.
141A.Hess JA, Hecker S. Workplace stretching programs: the rest of the story. Appl Occup Environ Hyg. 2003;18(5):331-8.
141B.Gartley RM, Prosser JL. Stretching to prevent musculoskeletal injuries. An approach to workplace wellness. AAOHN J. 2011;59(6):247-52.
142.Da Costa BR, Vieira ER. Stretching to reduce work-related musculoskeletal disorders: a systematic review. J Rehabil Med. 2008;40(5):321-8.
143.Marangoni AH. Effects of intermittent stretching exercises at work on musculoskeletal pain associated with the use of a personal computer and the influence of media on outcomes. Work. 2010;36(1):27-37.
144.Choi SD, Woletz T. Do Stretching Programs Prevent Work-related Musculoskeletal Disorders? J SH & E Research. 2010;6(3):8-24.
145.Bell JA, Burnett A. Exercise for the primary, secondary and tertiary prevention of low back pain in the workplace: a systematic review. J Occup Rehabil. 2009;19(1):8-24.
146.Brodal P. The Central Nervous System, Structure and Function. Oxford, NY: Oxford University press; 2004:251-264.
147.Gregory JE, Brockett CL, Morgan DL, Whitehead NP, Proske U. Effect of eccentric muscle contraction on golgi tendon organ responses to passive and active tension in the cat. J Physiol. 2002;538(pt 1):209-218.
148.Strom V, Knardahl S, Stanghelle JK, Roe C. Pain induced by a single simulated office-work session: time course and association with muscle blood flux and muscle activity. Eur J Pain. 2009;13(8):843-52.
149.Larsson SE, Alund M, Cai H, Oberge PA. Chronic pain after soft tissue injury in the cervical spine: trapezius muscle blood flow and electromyography at static loads and fatigue. Pain. 1994;57(2):173-80.
150. Hochanadel CD, Conrad DE. Evolution of an on-site physical therapy program. J Occup Med. 1993;35(10):1011-1016.
OTHER GREAT REFERENCES (some older, but still valid info)
Bullock, M., ed.: ERGONOMICS: THE PHYSIOTHERAPIST IN THE WORKPLACE, Churchill-Livingstone, 1991.
This landmark text describes the role of the physical therapist as the most qualified industry resource for ergonomics. The physical therapist is described as providing a valuable mix of musculoskeletal medical training with human biomechanics and physics of movement and posture as the basic science foundation of this profession. Most large industry settings in Europe employ on-site physical therapists as their ergonomics resource (in contrast with US industry which relies primarily on engineers.) In Scandinavian countries ergonomics is chiefly the domain of physical therapists. See pages 214-215 and 228-229.
pp52-53: Posture work load is described as a primary risk for CTD. Static muscle contraction reduces circulatory irrigation to muscle, decreasing oxygen and creating metabolic wastes accumulation in the tissues, leading to pain and hardening. Muscle posture work should not tolerate more than 5-6% of MVC in work conditions exceeding one hour. Rapid repetitive motion and high accuracy demands create increased background tensions in working muscles and tendons, as do noise and cold, creating similar stresses as seen in excessive posture load demands and high MVC. Similar stresses are seen when repetitive loading exceeds 50% of MVC and peak loading exceeds 75% of MVC. Similar stresses are seen in extreme positions and sudden jerky motions.
pp108-115: Posture load is described as a severe risk particularly in the presence of short rest breaks. Static posture loads with short rests is a strong risk. Posture load is a risk especially when posture is awkward or needed to manipulate tools distally. Speed of repetition increases static posture loads (Waersted 1986). Forward head posture is seen as a pain source in many static posture jobs according to one study, suggesting pain is a result of mechanical deformation of passive tissues (Harms-Ringdahl 1986).
…Static loading is identified as stress causing fatigue and reduction in blood flow at a time when wastes are increasing and oxygen demands are increasing (IBID). VDT work is discussed in this context, with up to 95% demonstrating symptoms (Bjorksten 1984). Management of this risk calls for improving posture habits, early symptom reporting, redeployment of work, and task alternation.
…Fatigue is the precursor to musculoskeletal pain problems. Repetitive light tasks produced significant changes in EMG and serum creatine kinase (SCK) in local muscles. These changes were not seen in heavy aerobic tasks (Hagberg and Jonsson 1982, 1984). The quality and frequency of rest affects the ability of muscles to recover (Rhomert).
pp134-143: Forward head posture produces stress through muscles posture load and passive tissue loads at ROM extremes, where EMG may be quiet. Posture loads at neck and shoulder are affected by motions, postures and loads in the arms and hands. Precision, speed, psychological stresses all increased muscle posture loads.
…Neutral upright head posture uses approximately 2% of MVC; slightly flexed uses 10%; much flexed posture uses 17% of MVC. Trapezius fatigue is reached where MVC is at 2-5% for more than an hour. This load is greatly increased with arm flexion or abduction. Flexion was defined as lower cervical flexion with some compensatory extension at upper cervical, a protracted head posture over the shoulders (Harms-Ringdahl and Schuldt 1988).
…Work with arms unsupported greatly accelerates fatigue. The more they are elevated, the more fatigue changes are seen spreading from the upper traps to the lower traps, thoracic erector spinae, rhomboids and glenohumeral muscles. Symptoms are related to time spent in forward postures, shoulder elevation, and total duration of arm activity. Endurance also depended upon the worker’s physical condition.
…Continuous arm activity entails no return to zero activity, so there is no relaxation of neck and shoulder muscles. Rather, movement is superimposed on static contractions. This is in light of the obstruction in perfusion of these working tissues (Schuldt, Jonsson, Christensen). The use of micro-pause loading breaks for only a few seconds are important to preserve comfort and work performance through the work day. When the hands and arms are supported during work activity, there is less pain in the neck and shoulder region(Hunting, 1981). Elbow support, properly designed, reduced activity in the traps, rhomboids, and erector spinae in both erect and flexed head positions among assembly workers (Schuldt, 1987).
pp310+ : Abstracts the papers used in the text. Extensive, highly pertinent information.
Hertling and Kessler: MGT OF COMMON MUSCULOSKELETAL DISORDERS, pp138-140, Lippincott, 1990.
Pages 138-140: These three pages from this landmark textbook offer a remarkably clear and detailed description of the pathogenesis of tendinitis and CTD at the cellular and molecular level Authors discuss the metabolic and nutrient pathways for tendons under work stress. It describes tendon breakdown in response stresses as a nutrient pathway problem, resulting in acute inflammation, fibrosis and eventual chronic inflammation. It describes the physical properties of tendon versus scar tissue and its ability to tolerate physical stresses. Vascularity and nutrient pathway is described as part of pathomechanics. Balance between rest and activity are discussed relative to work recovery. EXCELLENT!
Kelley, M., and Clark, William: ORTHOPEDIC THERAPY OF THE SHOULDER; Lippincott, 1995; Chapter 3, pp144-149.
These pages provide the very best available description of the various entities that comprise “thoracic outlet-inlet syndrome.” This is a highly controversial topic within the medical community, due to varying definitions of what really is thoracic outlet-inlet syndrome. These pages describe the varied entities that fall into this category, clarifying the various categories of disorders that may fall into this diagnosis. This is essential for the prevention specialist to understand in their work on workplace injury prevention and the role of the thoracic outlet-inlet.
Ellis, J.: “Balancing the Upper Quarter Through Awareness of RTTPB” CLINICAL MGT, Vol. 7, No. 6
Describes sources of posture dysfunctions for upper quarter problems. These include TMJ dysfunction, thoracic outlet syndrome, cervical strain, shoulder problems and headache. Implies a postural relationship among TMJ, neck pain and upper extremity problems. Describes restoration of erect upper body posture, correction of breathing mechanics and unloading TMJ stresses posturally as an essential treatment objective in upper quarter problems.
Jackson, P.: “Thoracic Outlet Syndrome: Evaluation and Treatment” CLINICAL MGT, Vol. 7, No. 6.
This paper describes TOS pathomechanics in details. Prior neck trauma and abnormal posture habits are identified as risk factors. Correction of posture habits and body mechanics are identified as foremost in treatment objectives. Correction of round shoulders slumped postures, scaleni stretching and relaxed diaphragmatic breathing are recommended.
Joyce, M.: “Ergonomics Will Take Center Stage in the 90’s and Next Century” JOR OCC HLTH AND SAFETY, Jan 1991.
The American Academy of Orthopedic Surgeons estimates repetitive motion injuries costs the US $27 billion annually for medical and lost salary costs. One risk is the young people entering the work force are less physically fit. This is combined with the increasing age of the worker population, bringing degenerative and disease risks with age.
Hansford, P.; et al: “Blood Flow Changes at the Wrist in Manual Workers After Preventive Interventions”: J HAND SURG: 1968: 11A: 503-508
Manual workers performing repetitive motion tasks were provided a five minute exercise program. Another group of workers were provided a five minute rest period. These interventions were performed after 1.5 hours of repetitive motion work tasks. Radial and ulnar artery blood flow were assessed with the Doppler method, as was Systolic blood pressure on the dominant extremity. Radial and ulnar blood flow velocity decreased while Systolic blood pressure remained stable after the 1.5 hours of manual work. Both the rest and exercise groups demonstrated increased blood flow velocity, unchanged radial blood pressure and decreased ulnar blood pressure. The five minute exercise group demonstrated greater increases in radial blood flow velocity than did the five minute rest group. Sustained, repetitive motion manual work can produce a decrease in blood flow through the wrists. Brief exercise programs have been shown to improve circulation at the wrist after circulation was compromised by the performance of manual work. Such programs may offer one practical method of preventing soft tissue injuries related to sustained compromise of blood flow at the wrist.
Allers, V.: “Workplace Preventive Programs Cut Costs of Illness and Injuries”; J OCCUP HEALTH & SAFETY: October 1989: 26-29.
Pre-work flexibility stretching exercises have demonstrated significant reductions in employee musculoskeletal injury and company health care costs. Warm-up stretching exercises were designed for employees in various work settings. These exercises emphasized flexibility throughout the spine, lower extremities and upper extremities. The objective of the exercises was to restore flexibility through passive stretching, improve blood flow to on-demand tissues and enhance fitnessand self-care attitudes among employees.
Renco Forest Products in Central Point, Oregon, demonstrated a 91% reduction in injuries after one year of pre-work stretching exercises on the job. Roseburg Forest Products of Roseburg, Oregon, reduced lost-time injuries by 80% in one year with this program. Smurfit Newsprint Corporation in Oregon City, Oregon, reduced lost-time injuries by 95% in three years since starting the program. Tigrad Care Center in Portland, Oregon, has reduced lost-time injuries by 78% and lost work days by 96%. J.M. Smucker’s Company of Woodburn, Oregon, reduced accidents during its six-month seasonal employment period by 56% and at cost savings of 95%.
HEBERT,L :”OSHA Ergonomic Guidelines and the PT Consultant,” PT MAGAZINE, Jul.95
This paper describes how stronger OSHA enforcement efforts against Worker Compensation claims for CTD and back injury represents a tremendous opportunity to physical and occupational therapists to offer their services to industry as injury prevention consultants. The OSHA Ergonomic Guidelines 3123 is described as a format for the consulting therapist to design and present a comprehensive prevention and ergonomics plan to client workplaces. The paper discusses in detail the complicating attitude and sociopolitical issues surrounding the controversy that often accompanies a CTD claims problem in the workplace. This is described as a primary avenue to follow in evaluating and designing a comprehensive prevention program. A specific ergonomic risk analysis checklist and recommendations report is presented as an example of the approach therapists may take.
HEBERT, L: “Cumulative Trauma Prevention” CLINICAL MGT, Vol 10, No 5, Sept-Oct 1990
Discusses in detail the format, content and rationale behind the IMPACC CTD School. Discusses the procedure of marketing and providing this service to industry. Describes protocol of Work Risk Analysis, management training, employee worksmart training, preventive exercises, task rotations.
HEBERT, L: “A Change of Place” CLIN MGT, VOL. 8, NO. 6
Discusses the role physical therapist may play as consultants to industry to help them learn how to understand and resolve their injury risk issues pertaining to low back and CTD claims. Describes the Back School and CTD School formats of prevention training in the workplace.
HEBERT, L: “Stretching Exercises in the Workplace” ORTHOP PT PRACTICE, Vol.11, no.4, 1999
Describes IMPACC stretching program for the workplace; strategies, specifics, outcomes.
HEBERT, L: “Becoming a Consultant to Industry” ORTHOP PT PRACTICE, vol.12, no.2, summer 2000
Profiles the services PTs may offer to industry as a consultant: prevention and treatment services. ergonomics, CTD School, Back School, on-site services, preferred PT provider arrangements, early intervention-primary care PT strategies.
HEBERT, L: “Analytic Focus to Preventing CTD” J OCCUP HLTH & SAFETY, Apr 1993.
Describes a comprehensive approach to identifying and correcting hazards for CTD. Describes a methods of Risks Analysis, Management Education, Employee Motivation Training and other tactics. Injuries, claims and costs are described as separate issues, each with its own prevention strategy. Describes the IMPACC CTD SCHOOL approach to implementing an effective program, particularly to overcome attitudes and workplace politics that make claims expensive.
HEBERT, L: “Body At Work; Preventive Stretching on the Job” J OCC HLTH SAFETY, pp48-58, Oct 1992.
This paper describes mechanisms of CTD, strategies for prevention, limitations of a strictly engineering approach to CTD prevention, and discusses design and rationale of a preventive stretching program for the workplace. Employers report significant successes with the plan developed by IMPACC physical therapists. Table illustrates several successful preventive exercise outcomes with reductions in CTD lost time days ranging from 60 to 98 percent in the year following, some with measured increases in productivity. Major feature of the described exercises is the consideration of proximal structures to be stretched, i.e. scaleni and other thoracic outlet-inlet tissues
One key feature of these exercises is stretching of the scaleni to open the thoracic outlet-inlet. Exercises and CTD prevention training program described in this paper have a ten-year experience history at nearly 300 companies throughout the US.
HEBERT, L. “A Cumulative Trauma School for Industry” INDUSTRIAL REHAB QUARTERLY, fall 1992
This article describes the format and strategy of the IMPACC CTD SCHOOL. Rationales, pathophysiology, and prevention strategies are explained. This article offers a table summarizing the successful outcomes of eleven companies that implemented the IMPACC CTD SCHOOL program.
HEBERT, L “Preventive Stretching Exercises” IND SAFETY & HYGIENE NEWS April 1992.
Preventive stretching exercises for the workplace are described. Outcomes and rationale are presented, describing successful programs.
HEBERT, L: “The Politics of Work Injury Prevention” IND SAFETY AND HYGIENE NEWS,May 1992.
Discusses preventing CTD to be more of a political issue than a safety issue, requiring management training and attitude adjustment prerequisite to ergonomic efforts and employee behavior changes. Proposes that while it is the responsibility of management to provide a safe workplace, it is the responsibility of workers to properly use and care for the working body. Describes socio-political issues IMPACC addresses in its training program, The CTD School
HEBERT, L: “New Opportunities for Physical Therapists in Industry” PHYS THER TODAY, Spring 1991
Describes the opportunities available to physical therapists to present themselves to industry as consultants on work injury prevention. Describes Work Risk Analysis services, Back School, CTD School programs for managers, supervisors and workers. Discusses marketing strategies.
Lutz, G.; et al: “Cumulative Trauma Disorder Controls: The Ergonomics Program at Ethicon, Inc.”: J HAND SURG: 1987: 12A (2,part 2): 863-866.
A ten-year experience history of an ergonomics task force for Ethicon, Inc. is described. The program is based on multiple strategies, including ergonomics, policy management, training and preventive exercise programs. Medical management procedures were developed for effective treatment and rehabilitation. Ergonomic design criteria for new and existing equipment were established. Employee orientation and education programs were provided to build acceptance of ergonomics and exercise strategies.
A preventive exercise program was established and studied. Exercises were performed twice per day per shift for approximately seven minutes each session. Participation level was voluntary, averaging between 80% – 90%. Prior to the exercise program, the medical department reported an average of 76 work-related visits for CTD problems per month. Following the exercise program, three months later, the medical department reported an average of 28 work-related visits per month for CTD problems. This is nearly 63% reduction in medical department visits for CTD-related complaints following initiation of a preventive exercise program.
Sawyer, K.: “An On-Site Exercise Program to Prevent Carpal Tunnel Syndrome”: PROFESSIONAL SAFETY: May 1987: 17-20.
Workers at a racquetball racquet manufacturing facility were experiencing a high frequency of carpal tunnel syndrome-related problems. From September 1983 until May 1984, 11 workers were referred for medical attention, two requiring carpal tunnel relief surgery. A preventive exercise program was initiated in July 1984. These exercises included stretching of various muscle groups in the neck, shoulders, arms and hands. Contract-relax exercises were provided for the fingers and thumb.
From July 1984 through May 1987, there had been only one case of carpal tunnel syndrome reporting for medical attention. This was successfully corrected with conservative treatment. It was noted that in May 1986, ergonomic modifications were made to some tools in a attempt to reduce forearm muscle work demand. Nearly two years of the exercise program had passed to that point.
Silverstein, B.; et al: “Can In-Plant Exercise Control Musculoskeletal Symptoms?”: J OF OCCUP MED”: Vol. 30, No. 12, Dec. 1988: 922-927.
After one year of an on-the-job exercise program to control musculoskeletal subjective symptoms in the neck and upper extremity, there were no statistically significant differences in localized posture discomfort. 67% of respondents who participated in the exercise program reported that the program made them feel better.
The exercises employed in this study included shoulder joint stretching and hand squeeze-relax to a bean bag. The author stated that any gain that might have been made with the exercise program may have been over shadowed by increasing productivity demands. The authors also pointed out on-going ergonomic problems with the jobs being studied.
{{ LAUREN’S RESPONSE: Exercise design was questionable. This did not demonstrate that exercises are iseless; this demonstrates that improper exercises are useless! Ergonomic stresses persisted uncorrected. Production demand increased. Confusing and contradictory conclusion statement stated there was no difference in discomfort, yet 67% felt better? }}
De Vera Barredo R, Mahon K: The effects of exercise and rest breaks on musculoskeletal discomfort during computer tasks: an evidence based perspective. J Phys Ther Sci, 2007, vol 19, no 2: 151-163. A review of research evidence on effects of exercise and rest breaks on musculoskeletal discomfort during computer work found that evidence supports use of rest breaks and exercise breaks to reduce discomfort. The evidence, in aggregate, suggests no additional benefits of exercises over rest breaks. This review identified widespread problems with research design, internal validity, statistical analyses, dropout rates and poor subject compliance. This serves to illustrate the potential value of rest breaks and exercise breaks but identifies problems with the research in allowing us to reach valid conclusions. This article is also an excellent demonstration of how to assess the value of research according to levels of evidence and internal validity.
Fenety A, Walker JM: Short-term effects of workstation exercises on musculoskeletal discomfort and postural changes in seated video display unit workers. Phys Ther, 2002, 82: 578-589. Authors examined short term effects of an exercise program on eleven subjects, involving an exercise break every 30 minutes. Exercises done by video display unit operators resulted in short-term decrease in both musculoskeletal discomfort and postural immobility. This is a non-randomized trial where participants acted as their own controls, resulting in evidence level IV with moderate internal validity.
Saltzman A: Computer user perception of the effectiveness of exercise mini-breaks. In: Proceedings of the Silicon Valley Ergonomics Conference and Exposition. Silicon Valley, CA, 1998, 147-151. Authors examined effects of an ergonomics exercise software program of frequent short stretch breaks. Participants reported stretch breaks were effective in reducing workplace discomfort. 23 percent of participants reported increased productivity. 34 percent of participants dropped out of the study. This study is level V evidence with weak internal validity.
**Thompson D: Effects of exercise breaks on musculoskeletal strain among data entry operators: a case study. In: Promoting Health and Productivity in the Computerized Office: Models of Successful Ergonomics Intervention. Taylor and Francis, 1990, 118-127. Employees were asked to perform five-minute exercise sessions during their two regular break periods. Operators reported reduced discomfort and generally improved physical condition. There were no Worker Compensation claims for one year into the program. Productivity had increased by 25 percent during the first four months of the program. Level of evidence is V, with weak internal validity.
***Karas B, Conrad K: Back injury prevention in the workplace: an integrative review. AAOHN J, 1996; 44(4): 189-96. Review of 15 experimental and quasi-experimental studies showed some positive evidence for back belts, back schools, stretching programs, and educational classes. Back schools and stretching programs were studied more frequently and showed the greater proportion of positive results.
***Moore T: A workplace stretching program. Physiologic and perception measurements before and after participation. AAOHN J, 1998, 46(12): 563-8. Participants who completed a structured stretching program had zero occurrences of MSD during the two-month period. There was statistically significant improvements in flexibility and the Fox Self Perception Profile, suggesting that flexibility exercises may reduce workplace MSD.
***Hess J, Hecker S: Workplace stretching programs: the rest of the story. Appl Occup Envir Hyg, 2003; 18(5): 331-8. Several studies are examined and analyzed in detail, describing positive and negative findings among a variety of studies and exercise approaches. One study review included flexibility program for firefighters. Showing no significant reduction in incidence of LBI, but injury costs significantly reduced ($85,372 for stretch group versus $235,131 for control group) from Hilyer 1990.
***Hilyer J, et al: A flexibility intervention to reduce the incidence and severity of joint injuries among municipal firefighters. J Occup Med 1990, 32(7): 631-637. A flexibility program for firefighters showed no significant reduction in incidence of musculoskeletal injury, but total injury costs significantly reduced ($85,372 for stretch group versus $235,131 for control group)
Rosta, P.: “Industrial Workers Excel With Work Hardening” REHAB MGT, April-May 1991.
Half of all workers injured on the job never return to work after six months of absence. 90% recover after 12 weeks. The remaining 10% account for 80% of costs. Companies rely on ergonomic redesign of work stations. This inadequate since there is no direct link between ergonomic design and high Worker Comp claims. A company’s Worker Comp problem is a complex set of economic, political, medical and legal issues. These must all be considered. Limiting attention to job design issues is putting a simple band-aid on a very large wound.
Melnik, M.: “Enlisting Participation in an Injury Prevention and Management Program” WORK, Fall, 1990.
…Various prevention approaches have been promoted in industry: ergonomic re-design, employee training, incentive programs, fitness and exercise plans, supervisor training, and psychosocial strategies. Most claim at least modest success. There appear to be several common themes that account for success: genuine management commitment, ongoing efforts to keeps programs alive, employee willingness to participate. Prevention programs are doomed to failure without the participation of all parties.
…Therapist consultants to industry must consider existing industry conditions that may affect outcomes: an existing medical management program, an effective return to work policy, official employee education system, equipment problem reporting system, official lines of communication, a physician who understands the job demands, relations between managers and supervisors, relations between supervisors and employees, and employee job satisfaction.
…Injury causes fall into two categories: conditions versus behaviors. Programs that focus just on job design will be helpful when such conditions are at risk, but industry must be aware that this addresses only one aspect of the problem. Buying ergonomic chairs does not reduce stress for an employee who does not use it correctly. Safe work is often a choice. Safe choices require education. Industry would be naive to believe they can eliminate all risk factors through design changes.
…The first step is to define unsafe conditions and unsafe behaviors. Unsafe behaviors are the result of: communication deficits, negative attitudes, poor physical condition, insufficient knowledge, stress, and lack of proper supervision. A truly effective program must address behaviors, attitudes, knowledge and physical condition along with the physical work environment.
…Essential components include: orientation of top managers, work site evaluation, a task force, employee education, supervisor education, address strength and flexibility, review sessions, an on-site stretching program, task force updates, and an incentive program.
Nag P, et al: Influence of arm and wrist support on forearm and back muscle activity in computer keyboard operation. Appl Ergo. 2009; 40(2): 286-291, Study examined muscle activity while using a wrist rest, forearm support and floating (unsupported) upper extremity work posture during keyboard work. Wrist rest showed mixed reductions in muscle activity, while forearm support showed widespread reduction in muscle activity compared to forearms unsupported.
Conlon C, Krause N, Rempel D: A randomized controlled trial evaluating an alternative mouse and forearm support on upper body discomfort and musculoskeletal disorders among engineers. Occup Environ Med. 2008 May; 65(5): 311-8. In engineers using computers more than 20 hours per week, a forearm support board may reduce right upper extremity computer use.
Remple D, et al: A randomized controlled trial evaluating the effects of two workstation interventions on upper body pain and incident musculoskeletal disorders among computer operators. Occup Environ Med. 2006 May; 63(5): 300-6.
Comparing ergonomics training only with training plus computer trackball with training plus forearm support revealed that training plus forearm support was effective in preventing upper body MSD among call center employees
Sheley, Elizabeth: “Preventing Repetitive Motion Injuries,” HRM MAGAZINE, Oct. 95. This article comes from the non-refereed professional journal of human resource managers in industry. It discusses the introduction of the IMPACC program of CTD prevention to several workplaces. It describes a three-step approach: work risk analysis to identify CTD risks, management training to build company and supervisor commitment and knowledge for identifying and correction risks, and employee self-protection training. The IMPACC program is specifically highlighted as being particularly effective in reversing CTD claims. Several companies using the IMPACC program revealed dramatic reductions in injury claims. Mike Strakal, PT, of Elkhart, Indiana and Lauren Hebert, PT, of Portland, Maine, were profiled as IMPACC providers, describing their techniques and success with the IMPACC program.
Jenkins, B: “Differential Diagnosis and Management of Neck Pain”: PHYSIOTHERAPY: August 1982: Vol. 68, No. 8: 253-255.
This paper describes various neurophysiological and biomechanical processes of neck and upper extremity pain and dysfunction. It discusses various treatment strategies. It provides a detailed description of pathology of various neck conditions.
Of particular note on CTD, this paper describes a central summation phenomenon whereby nociception originating from various neck tissues due to inflammation or mechanical irritation can lead to a background of subliminal sensory stimuli which can increase the central excitatory state. This can lower the threshold of pain for other peripheral lesions throughout the upper extremity and explain the apparent correlation between painful shoulder problems, tennis elbow and carpal tunnel problems in cervical problems. The contribution of the cervical spine must be considered carefully when presented with one or more of these symptom complexes.
This paper, therefore, presents one neurological explanation as to how various and multiple CTD problems throughout the upper quarter may be related to neck problems. This offers an explanation of the apparent strong relationship between neck pain problems and carpal tunnel syndrome and tendinitis distally in the arm.
^^Zacharkow, Dennis, “Sitting Posture: The Overlooked Factor in C.T.S.” ADVANCE FOR P.T., May 16, 1994
This paper describes in great detail and extensive literature references the role of sitting posture stress in the etiology of Carpal Tunnel Syndrome, primarily via thoracic outlet compression caused by forward head posture during sitting work tasks. Numerous studies are quoted citing the strong relationship between CTS and TOC and forward head posture. 64% of thoracic outlet patients had clinical evidence of CTS in one study (Novak, 1993); another showed virtually 100%. Another study (Glick, 1994) of 500 CTS patients showed 93% had minor to moderate underlying cervical radiculopathies.
Barrer, S.: “Gaining the Upper Hand on Carpal Tunnel Syndrome” JOURNAL OCC HLTH AND SAFETY, Jan 1991.
CTD accounts for 48% of claims, up from only 18% less than a decade ago. This is a function of the shift to automation, requiring more repetitive motion in sustained postures. Repetition without adequate recovery leads to inflammation. NIOSH found that 8-9 repetitions per minute did not allow enough recovery time between repetitions to produce adequate lubrication of moving tissues.
The average high risk workplace will spend $250,000 on these claims per 100 employees per year (1988 dollars). The hidden costs are likely much greater: damage to morale, for one. Worker who feel the company is not responding adequately to the problem feel trapped and demoralized, possibly adding t the problem.
The first step is not to deal with at-risk workers. Rather, one must first educate management. It is imperative that top management become committed experts on the issues. The attitude of management will dictate the effectiveness of any prevention efforts. Only then should one proceed with employee training. Employee training is essential to ensure their working future. They must conform to company risk reduction policies, including on-the-job exercises.
Seater, S.: “Physical Therapy Emerging As a Partner in the Corporate Fight To Contain Costs” P.T. FORUM, Vol. 5, No. 13
Several examples of successful injury prevention and cost reductions following physical therapy consulting for injury prevention are cited. Westmoreland Coal reduced back injury lost days by 330, saving $53,130 in employee pay and benefits alone. Black and Decker reduced medical department visits by 50% with work station modifications and posture education from a P.T. Adoph Coors Beer used a P.T. to create a wellness and prevention program that saved them $663,677 in health costs alone. Lockheed Missile reduced back injuries dramatically with a back injury prevention training program. Public Service of New Hampshire reduced back injuries by 60% following a similar training process, as did Texas Instruments. Physical therapists are described as leading authorities on injury prevention due to their mix of training on musculoskeletal function, making them ideally suited to prevention programs emphasizing ergonomics.
Twomey, L. “A rational Approach to the Treatment of Back Pain by Manual Therapy” PHYS THER, Vol. 72, No. 12, Dec 1992
This author provides an excellent description of the pathophysiology of lower back degeneration and injury, describing the loss of nutrient pathway and physical changes due to sustained loading/strain stresses to articular cartilage and discs and ligament structures. The author discusses flexion loading, particularly sustained, as a mechanisms of injury and degeneration due to nutrient pathway changes, fluid dynamics, collagen and cartilage effects. End-range loading, creep and crimp effects are discussed. The role of passive extension and pause stretching to prevent injury and reverse many of these processes is described. Excellent discussion of prevention rationales.
McKenzie, R.: THE LUMBAR SPINE, MECHANICAL DIAGNOSIS AND THERAPY, Spinal Publications, 1981.
The McKenzie low back care manual. The standard reference on McKenzie protocol, lordosis lifting methods and mechanisms of disc injury. Extensive description of mechanisms of disc failure pp16-21.
Hart, D. et al: “Effect of Lumbar Posture on Lifting” SPINE, Dec. 1986.
This LANDMARK research dissertation compares various methods of lifting techniques and implications for avoiding back injury on materials handling tasks. Strictly controlled study shows the best method to be one of maintaining lumbar lordosis during squat lifting. This method is demonstrated to be favored over the traditional “pelvic tilt” method.
Lumbar flexion moments were least in this lifting posture. Protective muscle recruitment of erector spinae and obliques was highest with this lifting posture, particularly during the critical early stage of the lift. An extensive and valuable bibliography is provided.
Delitto, R., et al: “EMG Analysis of Two Techniques for Squat Lifting” PHYSICAL THERAPY, Vol. 67, No. 9. Sept 1987.
This study describes the effects on the spine for two different methods of squat lifting: pelvic tilt versus maintaining lordosis. The researchers discovered that for pelvic tilt, flexion moment loads were at maximum at the beginning of the lift while protective contractions of erector spinae and abdominal obliques were at minimum. During lordosis lifting, protective activity of the erector spinae and abdominal obliques was highest at the critical early stage of lifting. It was concluded that lordosis lifting method offered the best potential muscle protection, particularly during the critical early phase of the lift.
One of the best papers re motor activity of ES during flexion and lifting in various postures. Reveals near shutdown of erector spinae and abdom obliques (needed to stabilize and protect LB structures during lifting) when lifting done with LB flexion, but high activity during lifting with lordosis preserved. A landmark paper validating maintaining lordosis during squat lifts (per McKenzie) to recruit active muscle protection of passive tissues during loading.
Lepore, B. et al: “The Dollars and Sense of Occupational Back Injury Prevention Training” CLINICAL MGT, Vol. 4, No. 2
1000 Lockheed Missile and Space Co. employees participated in a back injury prevention training program that resulted in a 67.5% reduction in total back injury liability costs, a 71% reduction in lost time cases for back injury, a 76% reduction in costs per case, and a 57% reduction in injury cost reserves.
Gatty C, et al: The effectiveness of back pain and injury prevention programs in the workplace. Work 2003; 20(3): 257-66.
Review of nine studies showed that positive outcomes were associated with studies reporting high compliance that used job-specific and individualized/small group education and training approaches.
Schenk R, Doran R, Stachura J: Learning effects of a back education program. Spine 1996; Oct 1; 21(19): 2183-2189.
The American Back School was compared to a video education group and a control group. Learning effect was assessed by examining gains in post-test results. No differences in post-test comparisons were seen in control and video groups. Significant differences were seen in the back school group at the .001 level, indicating that back school is an effective intervention for influencing lifting posture and conveying information on spinal mechanics and lifting technique. Additionally, video training may not be an effective prevention intervention.
Heymans M, van Tulder M, et al: Back schools for nonspecific low back pain: a systematic review within the framework of the Cochran Collaboration Back Review Group. Spine. 2005; 30(19): 2153-63. There is moderate evidence suggesting back schools in an occupational setting reduce pain and improve function and return-to-work status.
Karas B, Conrad K: Back injury prevention in the workplace: an integrative review. AAOHN J, 1996; 44(4): 189-96. Review of 15 experimental and quasi-experimental studies showed some positive evidence for back belts, back schools, stretching programs, and educational classes. Back schools and stretching programs were studied more frequently and showed the greater proportion of positive results.
Hickey, D., et al: “Relation Between the Structure of Annulus Fibrosus and Function and Failure of Intervertebral Disc” SPINE, Vol. 5, No. 2
Annulus fibers have the same mechanical properties as tendon fibers, per tolerance to stretch and strain. Failure of the annulus is most likely to fail during forward bending loads and during torsion loads. Compression is more likely to cause end-plate failure. {This paper is often cited as one basis for not advocating pelvic tilt lifting methods.}
McGill, SM: “Low Back Exercises: Evidence for Improving Exercise Regimens” PHYS THER, Vol. 78, No. 8, Aug 1998. pp 754-765.
An exceptional laboratory analysis of various exercise methods, lifting techniques, injury mechanisms, including a rare incident that produced a video fluoroscopy of an instability injury as it occurred. A wealth of valuable information on lumbar injury and care is provided in this article. Well-supported suggestions for exercises.
Byl, et al: “A Primate Model for Studying Focal Dystonia and Repetitive Strain Injury: Effects on the Primary Somatosensory Cortex,” PHYSICAL THERAPY, Vol 77, No 3, Mar 1997
This study illustrates changes in the brain as a result of repetitve motion demands at the hand. Repetitive hand motion degrades hand representation in the sensorymotor cortex of the brain and interferes with motor control. Restoring hand representation may be a critical part of treatment for patients with RSI.
Solomonow, M, et al “Increased Exposure to Lumbar Injury due to Cyclic Loading,” Volvo Award, presentation at Intl Soc for Study of Lumbar Spine, as yet unpublished, 1999.
Repetitive mechanical loading progressively desensitizes mechanoreceptors in soft tissues of the spine. This results in exponential decrease in protective reflex muscle activity, increasing risk of injury. Discs, ligaments and other viscoelastic structures progressively deform (creep) under such repetitive loads, as muscles lose their ability to stabilize the spine from fatigue, mechanoreceptor desensitization and neurological habituation. Rest periods required hours to recover lost tension in experimental tissues (feline model)…
McGill, Stuart, “Invited Commentary” , JOSPT, vol 30, no 5, May, 2000
Exceptionally enlightening commentary on the above two articles, in perspective with several other related studies, noting how all these fit the realities of the workplace (prevention) and clinic (rehabilitation). Excellent bibliography. Summary findings include: Continuous lifting is the more valid function to examine; Experienced lifting workers will use a variety of lifting postures throughout the work day; Curvature of lordosis important to control lines of action along many lumbar stabilizer muscles, more beneficial mechanically than lumbar flexion positions; Spine ROM and strength have little correlation with future injury; Use of screening measures legally risky and very limited; Patients should be classified functionally and by specific injured tissues to determine lifting technique.
Byng J: Overuse syndromes of the upper limb and the upper limb tension test: a comparison between patients, asymptomatic keyboard workers and asymptomatic non-keyboard workers. Man Ther 1997, 2: 157-164
The ULTT was positive in 100 percent of the patient group, supporting the hypothesis that the pathology of occupational upper limb overuse is neurogenic in origin. Furthermore, the asymptomatic keyboard users (intended to be a control subgroup) also had a significantly higher positive ULTT compared to asymptomatic non-keyboard users (the other control subgroup).
Lundborg G, Dahlin L: Anatomy, function, and pathophysiology of peripheral nerves and nerve compression. Hand Clin 1996; 12(2):185-93.
The clinical stages of nerve compression lesions can be related to changes in intraneural microcirculation and nerve fiber structure, alterations in vascular permeability and subsequent formation of edema. The double crush and reverse double crush syndromes are related to disturbances in axonal transport induced by compression, followed by morphological and functional changes in nerve cell bodies.
Edgelow P: Ch.6; Neurovascular consequences of cumulative trauma disorders affecting the thoracic outlet: a patient-centered approach. In Donatelli R (ed): Physical Therapy of the Shoulder; 1997; Churchill-Livingstone.
Comprehensive description of pathomechanics and pathophysiology of thoracic outlet compression.
BACK BELTS …Kraus, Jess, et al: “Reduction of Acute Low Back Injuries by Use of Back Supports,” INTL J OCCUP & ENVIR HLTH, Oct-Dec 1996, Vol. 2 (3).
This paper is a well-controlled study of the effectiveness of low back support belts in reducing low back injuries. The study was sponsored by UCLA School of Public Health and the Southern California Injury Prevention Research Center as an objective study independent of the back support industry. The study of 36,000 employees at 31 Home Depot stores in California encompassing 101,000,000 work hours revealed a decrease of 34% in low back injuries following a mandatory policy on use of back supports among employees. Favorable effects were seen in both genders, young and old, new or experienced workers, low lifting intensity and high lifting intensity jobs. The study provides scientific evidence that proper use of back supports as part of a comprehensive back injury prevention program. can be effective in reducing back injuries.
BACK BELTS .. Kraus, J, et al: “Back Supports & Low Back Injuries: a Second Visit with the Home Depot Cohort Study Data”, INT J OCCUP ENVIRON HEALTH, 1999, 5:9-13
This paper revisits data for the study demonstrating significant favorable effects of wear back supports in the workplace, to answer the firestrom of criticism from ergonomics professionals seeking to discredit the report. All the questions raised were examined and assessed for validity and objectivity. All issues were fully answered, reinforcing the validity of the findings that back supports did indeed reduce back injury lost days by 34% among 36,000 Home Depot employees over a six year period.
BACK BELTS .. Allen, S.K. and Wilder, K. “Back belts pay off for nurses”, Occ. Health & Safety, 65 (1) (1996) 59-62.
back belts – the general use of back belts in the distribution industry has been questioned. However, in a study of 47 employees over a 6-month period, the use of back belts significantly reduced injury risks. The test group with back belts worked 22,243 hours and had no injuries, whereas the control group worked 23,109 hours and lost 80 hours due to back injuries
BACK BELTS .. Warren, L, et al, “Effects of Soft Lumbar Support Belt on Abdominal Oblique Muscle Activity in Nonimpaired Adults During Squat Lifting” J ORTHOP SPORTS PHYS THER, June, 2001; 31
Wearing a soft lumbar support during squat lifting significantly decreases activity of abdominal obliques. This study shows back belts reduce muscle activity and this should be consistent with decreased loads on the spine, likely due to increased intra-abdominal pressure. This is consistent with other studies that, taken together, demonstrate the both abdominal and back muscles produce less force during lifting with a back support. Decreased coactivation of the muscles around the spine suggests that spinal compressive forces are decreased. Loads on the spine during lifting tasks are positively correlated with increased muscle activity. Intra-abdominal pressure is significantly increased with wearing a back belt during lifting. Increased intra-abdominal pressure is believed to result in decompression of the spine during loading and decreased load on spinal muscles. There is also an increased recruitment of quadriceps muscle action during lifting with back belts, suggesting they encourage improved lifting technique.This paper mentions numerous studies in its text and its bibliography that add support to the hypothesis of the authors.
BACK BELTS .. Giorcelli RJ, et al: “TTHE EFFECT OF WEARING A BACK BELT ON SPINE KINEMATICS DURING ASSYMETRIC LIFTING OF LARGE AND SMALL BOXES” SPINE, 2001;26(16):1794-8.
28 subjects with at least six months’ materials handling experience and no histories of low back pain were involved in structured lifting tests, wearing the flexible back support and not wearing it. The research evaluated the effect on spinal kinematics (flexion, right and left bending, and right and left twisting, and lifting velocity) on experienced materials handlers wearing no-suspenders, flexible back supports (“belts”) and lifting both small and larger boxes. Their results indicated that, under most test conditions, the “subjects with belts lifted more slowly and used more of a squat-lift technique, regardless of box size. Belts reduced more torso motions while lifting large boxes.” Further, they state that, “belt use significantly affected spine kinematics by decreasing maximum spine flexion, maximum spine flexion angular velocity, maximum spine extension angular velocity, maximum torso left lateral bending velocity and maximum torso right lateral bending, and maximum torso left twisting for lifts with the large box.” These findings indicate that belts offer the worker the reminder to lift object in a less-risky manner (less flexion and more deliberate movement), something previous research has been advocating for years. The authors were not willing to draw the conclusion themselves, but their results indicate that, under the test conditions, the belts offered workers a substantial protective effect. The flexible back support they tested was associated with subject behavior that has been shown to be protective against low back pain and injury.
^^ D M Rempel, “A randomized controlled trial evaluating the effects pain of two workstation interventions on upper body pain and incident musculoskeletal disorders among computer operators” Occup. Environ. Med. 2006;63;300-306
Forearm Support Reduces Pain among Computer Users… A simple workstation modification, the addition of a forearm support, was found to reduce upper body pain and prevent musculoskeletal disorders among customer service workers who use a computer for more than 20 hours per week. In this randomized controlled trial, the 182 participating workers were followed for 1 year. Based on a cost-benefit analysis, employers could see a full return on the cost of providing arm boards to all employees within 11 months of the investment. The Morency rest forearm supports are manufactured by R&D Ergonomics of Maine. The study received the 2006 International Ergonomics Association/Liberty Mutual Prize
MacDermid,J., “Clinical & Electrodiagnostic Testing of carpal Tunnel Syndrome”, JOSPT, OCT 2004
Excellent review of various simple non-invasive diagnostic testing for CTS, with correlations to Electrodiagnostic testing. Includes highly valid testing per history, sensory screening, provocation tests, NVC-EMG.
Michlovitz, S., “Conservative Interventions for CTS,” JOSPT, OCT 2004
Excellent review of current PT approaches to clinical management of CTS.
Lee, M, “Pronator Syndrome and Other Nerve Compressions That Mimic CTS,” JOSPT, OCT 2004
Differential assessment of median nerve compressions of the upper extremity proximal to the wrist, mimicking CTS, along with treatment approaches for these.
Barr, A, “Work-Related Musculoskeletal Disorders of the Hand and Wrist,” JOSPT, OCT 2004
Epidemiology, pathophysiology and sensorimotor changes are reviewed. Reviews many studies. Of particular note is the description of pathophysiology, especially describing histochemical changes that can trigger inflammatory responses systemically. Cytokines are released from local inflammatory sites may trigger systemic inflammatory responses, thus causing tendinitis symptoms to spreading to other sites. Of equal interest is the motor behavior degradation that can occur with repetitive motion tasks, causing loss of motor control and a resulting loss of coordination and movement efficiency that may increase work damage. This may be the result of changes at the brain where repetitive movement causes degradation of motor cortex, distorting motor control. This is reorganization of CNS control of movement.
^^ Novak, C, “Upper Extremity Work-Related Musculoskeletal Disorders: a Treatment Perspective,” JOSPT, OCT 2004
This is an excellent discussion of various important pathomechaics of MSD. Of particular interest is the prevalence of multi-level neurovascular compressions (double-crush) {{a critical issue in prevention tactics where we address proximal posture risks to reduce distal repetitive motion problems}}. Static postures, particularly at the neck are also described {{another critical issue in prevention tactics where we address proximal posture risks to reduce distal repetitive motion problems}}. Posture risks at various articulations are described. Treatment approaches are also well-described in this paper.
Barr, A, Barbe, M: Pathophysiological Tissues Changes Associated with Repetitive Movement: A Review of the Evidence. Phys Ther. 2002 February: 82(2): 173-187.
This article presents several key considerations defining MSD pathophysiological mechanisms taken from extensive literature review, particularly among animal studies describing neuromusculoskeletal responses to repetitive or sustained loading demands. Key points include:
CELLULAR CHANGES:
Muscle tissue biopsies of humans with hand overuse symptoms showed histological and muscle fiber structure changes consistent with denervation or ischemic loss of type II fibers with hypertrophy of type I fibers. Upper trapezius samples showed changes consistent with hypoxia and reduced blood flow. Structural damage to tissues usually stimulates proliferation of progenator cells of that tissue. Cell membrane damage releases intracellular factors that stimulate infiltration of lymphocytes and macrophages. These processes stimulate regreneration, or scarring if that damage is ongoing. In tendons this can result in fibroblast proliferation leading to fibrosis and collagen dysplasia within the extracellular matrix.
Ongoing mechanical or metabolic stress such as hypoxia, ischemia or inflammation leads to release of heat shock proteins (HSP) by cells such as neurons, glia, fibroblasts and muscle cells. This is a healing protective response whereby these HSP restore denatured proteins. HSP are stimulated by ischemia or tears in cell membranes releasing cytotoxic free radicals. Cell damage releases cytokines, mediators of inflammation, cell proliferation and regeneration. Cytokines are proinflammatory proteins including interleukins, tumor necrosis factor (TNF), COX2 and prostaglandin. These mediate proliferation of macrophages and fibroblasts. The phagocytic action of the macrophages can further increase damage and release more cytokines, thus creating a vicious cycle of chronic inflammation. Damaged cells release chemicals that damage more cells. This cycle is prolonged and magnified when exposure to repetitive tasks is ongoing.
CNS CORD CHANGES:
Chronic pain can lead to neuroplastic changes in nerves, cord and cortex. Sustained nociception afferent bombardment can increase release of excitatory neurotransmitters glutamate and substance P within the dorsal horn. These can activate and potentiate synapse activity both presynaptically and postsynaptically. This can also alter genetic expression in neurons to upregulate receptor sites. The end result is hyeralgesia (increased sensitivity to nociception) and allodonia (non-painful stimuli felt as pain). Clinicians often mistake this process as “symptom magnification” or psychological complications. Nerve constriction peripherally due to repetitive or sustained mechanical compression can also cause neuroplastic changes in the dorsal root ganglion that can increase nociception transmission.
CNS CORTEX CHANGES:
Repetitive tasks can induce changes in cerebral cortex, particularly de-differentiation of cerebral cortex representation of the hand. This is induced by constrained and repeated motions at the upper limb. Loss of specific hand field representation of the cortex causes loss of coordination and changes in movement behaviors toward less efficient motor control. This loss of movement efficiency increase fatigue and pain risks during repetitive tasks. This is maladaptive movement behavior. It may be that this motor control degradation precedes the onset of pain and may even precipitate it.
SYSTEMIC INFLAMMATORY REACTION
Animal studies of this phenomenon revealed increased cellular chemical changes described above: increased HSP-72, COX2, and macrophage infiltration at levels 1000 times above baseline. BUT of particular note… these biochemical changes were seen also in the non-moving control limbs, suggesting a systemic inflammatory response to the high repetition low load tasks in the experiment. This suggests that repetitive task work can lead to not only local inflammatory reactions at the exposure site, but also leads to a wider systemic inflammatory response as well as neurological reorganization (neuroplasticity) centrally at the spinal cord, increasing nociception, and at the cerebral cortex, causing motor control degradation.
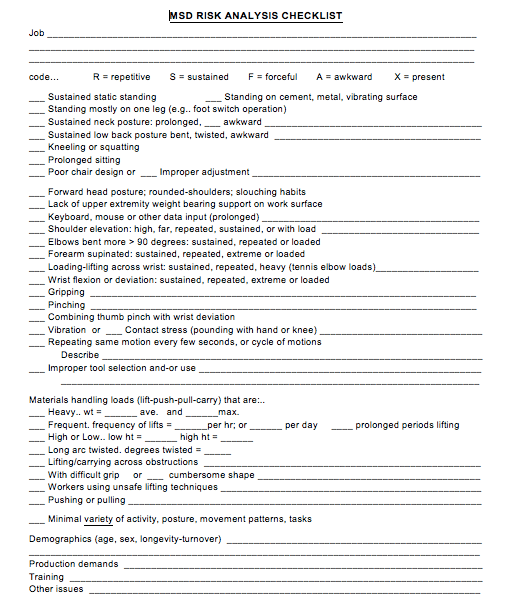


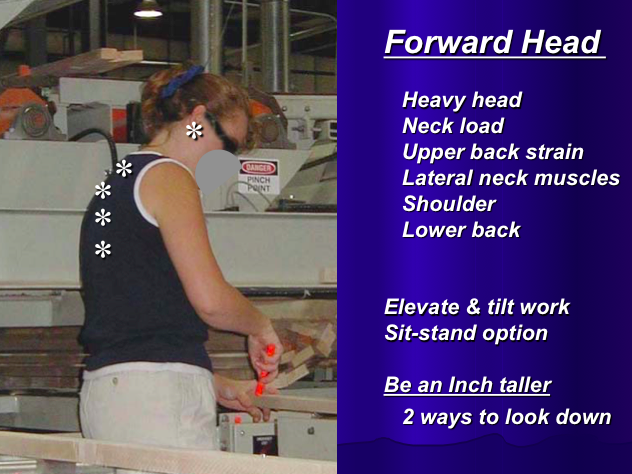 m
m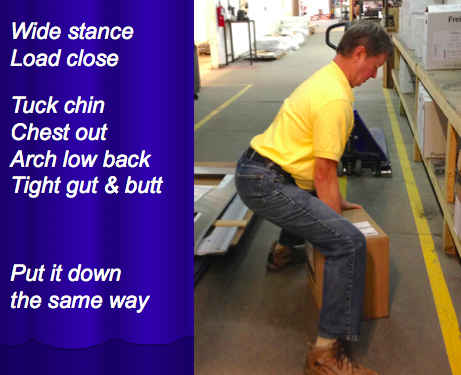 m
m